Archived Content
2023 (May 3-5) Rochester, MN Annual Meeting
Program
| 8:00 | Welcome by ACS President and Annual Meeting Program Chair |
| 8:15 | Claude P. Brown Honorary Lectureship Ronald C. Petersen, MD, PhD, Alzheimer’s Disease Diagnosis in the Era of Biomarkers |
| 9:00 | Sean Pittock, MD, Biomarker Discovery in Autoimmune Neurology: From the Dark Room to Near Cure! |
| 9:30 | Maria Willrich, PhD, Kappa Immunoglobulin Free Light Chains as an Alternative to Oligoclonal Banding for Diagnosis of Multiple Sclerosis |
| 10:00 | Break |
| 10:30 | Wolfgang Singer, MD, Towards Laboratory Biomarkers for Multiple System Atrophy and other Synucleinopathies |
| 11:00 | Anne E. Tebo, PhD, Biomarkers for systemic autoimmune diseases with neurological involvement |
| 11:30 | Session adjourns |
| 12:00 | Luncheon Seminar: Melissa Murray, PhD, From Microscope to Bedside: How Postmortem Observations Can Impact Biomarker Research |
| 12:45 | Break |
Session Theme: Artificial Intelligence in Medicine |
|
| 1:00 | Jason Hipp, MD, PhD, Computational Pathology and Artificial Intelligence |
| 1:30 | David McClintock, MD, Creating Strategies for Artificial Intelligence in Laboratory Medicine |
| 2:15 | Rickey Carter, PhD, Kidney Stone Spectral ID by Artificial Intelligence |
| 3:00 | Break |
| 3:30 | Ryan Robetorye MD, PhD, Developing genomic tests that guide large B-cell lymphoma diagnosis and treatment: Lymph2Cx and Lymph3Cx assays |
| 4:00 | Surendra Dasari, PhD, Faster and More Accurate Amyloid Subtyping Informatics |
| 4:30 | Mark Zarella, PhD, Operationalizing AI for Pathology Clinical Practice |
| 5:00 | Zeynettin Akkus, PhD, AI-Empowered Rapid Onsite Evaluation of Biopsy Specimens |
| 5:30 | Session adjourns |
| 6:30 | Musicale Rehearsal |
| 7:00 | Young Fellows Social (open to all young scientists ≤ age 45, regardless of whether a member of ACS and accompanying persons), hosted by Chris Crutchfield, PhD, for the Young Fellows Section, and Members of the Executive Committee |
Friday, May 5 |
|
| 7:55 | Joshua A. Bornhorst, PhD, Welcome and Announcements |
| 8:00 | William Morice, MD, PhD, Overview of Mayo Clinic Department of Laboratory Medicine and Pathology and Mayo Collaborative Services |
| 8:30 | Bobbi Pritt, MD, AI Detection of Parasites in Stool Samples |
| 9:00 | Break |
| 9:15 | Paola Ramos, PhD, Advances in Biobanking: Samples Collection, Processing and Storage |
| 9:30 | Stephen Murphy, PhD and Yifei Yang, PhD, Seeding and Accelerating Diagnostic Innovations at Advanced Diagnostics Laboratory |
| 10:00 | Angela Reese-Davis and Aaron Getchell, MBA, Overview of Specimen Operations – Team of One Video. |
| 10:15 | Session adjourns |
| 10:30 | Laboratory Tours · Anatomic Pathology – Hilton 3 · Central Clinical Lab/Central Speciality Lab – Hilton Court Level · Clinical Genome Sequencing Lab – Hilton 5 · FISH – Hilton 9 |
| 11:45 | Plummer Historical Suite Tour (self-guided) |
| 12:15 | Heritage Hall Tour (self-guided) |
| 12:45 | Rochester Trolley transportation |
| 1:00 | Lunch and Tour of Mayowood |
| 2:30 | Historic Trolley Tour |
| 4:00 | Trolley Tour adjourns |
| 4:15 | Gonda Building Tour (self-guided) |
| 6:15 - 10:00 | Ground Transportation to and from Foundation House |
| 6:30 | Annual Reception and Awards Banquet, Black Tie Optional, Christopher Crutchfield, PhD, Master of Ceremonies |
Banquet Speaker, W. Bruce Fye MD, MA, The Origins and Evolution of the Mayo Clinic from 1864 to 1939: A Minnesota Family Practice Becomes an International "Medical Mecca" |
|
| 10:00 | Banquet adjourns |
Saturday, May 6 |
|
| 8:00 | Edward Creagan, MD, The Burnout Pandemic: Proven Insider Tips to go the Distance |
| 9:00 | Jessica Claus, Beyond the scope: A comparative look at pathology education in the US and European medical schools |
| 9:45 | Sarrah Lahorewala, Assessing reliability of creatinine-estimated glomerular filtration rates in living kidney donor candidates |
| 10:00 | Break: Coffee and poster set-up |
At-Large Abstract Session Theme: Advances in Genetic and Biochemical Testing |
|
| 10:30 | Andy Nguyen, Deep learning predicts breast cancer HER2 status but not hormone receptor status |
| 10:45 | Shuko Harada, Effect of New Panel and Electronic Order on Solid Tumor NGS Testing |
| 11:00 | Anthony Maus, In-solution ion pairing benefits measurements, instruments, and the environment |
| 11:15 | Susan Ashrafzadeh-Klan, FGF23 assays: analytical and clinical considerations |
| 11:30 | Frederick Kiechle, Dengue fever in three countries and associated seroprevalence of Chikungunya and West Nile Virus |
| 11:45 | Session adjourns |
| 12:00 | Luncheon: Annual ACS Business Meeting, all faculty and attendees are invited regardless of whether members |
| 1:30 | Business meeting adjourns |
At-Large Abstract Session Theme: Lymph and Thyroid Evaluation |
|
| 1:30 | George Chen, The role of Nrf2 in differentiation and dedifferentiation of thyroid cancer |
| 1:45 | Diana Treaba, Lymph node development of dendritic CD10 positive stromal cells in aggressive B-cell lymphomas – friend or foe for lymphoma expansion? |
| 2:30 | M. John Hicks, Multifocal Follicular Adenomas of Thyroid Discovers PTEN-Hamartoma Tumor Syndrome in Children |
| 2:45 | Stephanie Barak, A rare case of metaplastic thymoma presenting with myasthenia gravis |
| 3:00 | Poster Session with Refreshments |
| Poster 1 | Charbel Abou-Diwan, Performance Evaluation of a High-sensitivity Assay for Serum Neurofilament Light Chain |
| Poster 2 | Rozeen Badeel, Intranasal plasmacytoma with anaplastic features and CIC and MCL1 alterations |
| Poster 3 | Christine Yu, An acute myeloid leukemia mimicker - plasma cell myeloma with a “blast-like” morphology |
| Poster 4 | Seul Byeon, Development of a diagnostic assay for Barth syndrome using mass spectrometry |
| Poster 5 | Hallie Walsh, Can the newest generation mass spectrometers eliminate the need for microflow LC? |
| Poster 6 | Ronald Phillips, Ovarian carcinosarcoma with a malignant squamous component: a case repor |
| Poster 7 | Richard Lahr, Distinguishing Delta-8 from Delta-9 Isomers in Tetrahydrocannabinol and Carboxy-Tetrahydrocannabinol |
| Poster 8 | Yahya Abdulrahaman, Dried Blood Spot Collection for AQP4-IgG testing provides opportunity for improving global health NMOSD diagnostics |
| Poster 9 | Jessica Claus, Unraveling the mystery of fatal eosinophilic pulmonary vasculitis in a neonate |
| Poster 10 | Charbel Abou-Diwan, Estimates of N-terminal pro-B-type Natriuretic Peptide Biological Variation from Eight Healthy Turkish Women |
| 4:10 | Poster Session Ends |
At-Large Abstract Session Theme: Reports of Interest |
|
| 4:15 | M. John Hicks, Primary Intraosseous Rhabdomyosarcoma: Rare Subtype Involving Mandible with Unique Translocation |
| 4:45 | Jessica Claus, An emerging danger for the pregnant population - A case of congenital syphilis |
| 5:10 | Session adjourns |
| 7:30 | Annual Musicale and Art Show, with reception |
Speaker Profiles

Ronald C. Petersen, Ph.D., M.D.
Professor of Neurology, Cora Kanow Professor of Alzheimer’s Disease Research
Director, Mayo Alzheimer’s Disease Research Center, Mayo Clinic College of Medicine
Dr. Ronald C. Petersen received a Ph.D. in Experimental Psychology from the University of Minnesota and graduated from Mayo Medical School in 1980. He completed an internship in Medicine at Stanford University Medical Center and returned to the Mayo Clinic to complete a residency in Neurology. That was followed by a fellowship in Behavioral Neurology at Harvard University Medical School/Beth Israel Hospital in Boston, Massachusetts. Dr. Petersen joined the staff of the Mayo Clinic in 1986 and became a Professor of Neurology in 1996. In 2000 he was named the Cora Kanow Professor of Alzheimer’s Disease Research and Mayo Clinic Distinguished Investigator in 2011. He is currently the Director of the Mayo Alzheimer’s Disease Research Center and the Mayo Clinic Study of Aging and has authored over 1000 peer-reviewed articles on memory disorders, aging, and Alzheimer’s disease.
Dr. Petersen is one of the recipients of the 2004 MetLife Award for Medical Research in Alzheimer’s Disease and the 2005 Potamkin Prize for Research in Picks, Alzheimer’s and Related Disorders of the American Academy of Neurology. In 2012 he received the Khachaturian Award and the Henry Wisniewski Lifetime Achievement Award in 2013 from the Alzheimer’s Association. In 2011 he was appointed by the Secretary of Health and Human Services to serve as the Chair of the Advisory Committee on Research, Care and Services for the National Alzheimer’s Disease Plan, and in 2014, he was appointed to the World Dementia Council by the UK government. In 2021, he was given the Lifetime Achievement Award for Alzheimer’s Disease Therapeutic Research.

Edward Creagan, MD, FAAHPM, will speak on The Burnout Pandemic: Proven Insider Tips to Go the Distance.
Dr. Creagan is a cancer specialist who practiced at the Mayo Clinic for more than forty Minnesota winters until his transition from clinical practice in late 2018. He was the first Mayo Clinic consultant to be board certified in hospice and palliative medicine. Dr. Creagan received the Distinguished Clinician Award, Mayo's highest honor and has served as president of the Mayo Clinic staff.
As an accomplished speaker, his presentations to both professional and consumer audiences are notoriously funny yet filled with useful lifestyle information. His main topics include survivorship, how to cope with burnout and stress especially in the time of COVID, the healing power of pets, and how to live long enough to cash in your 401(k).
In 2015, he received the Ellis Island Medal of Honor for contributions to descendants of immigrants.
He is the author of the triple award-winning book, How Not to Be My Patient: A Physician’s Secrets for Staying Healthy and Surviving Any Diagnosis and the equally award winning: Farewell, which provides answers to the vital end-of-life questions patients and families ask. Each of these were best sellers on Amazon.

W. Bruce Fye, MD, MA, will speak on The Origins and Evolution of the Mayo Clinic from 1864 to 1939: A Minnesota Family Practice Becomes an International “Medical Mecca”
W. Bruce Fye received his BA and MD degrees from Johns Hopkins, where he was elected to Phi Beta Kappa and Alpha Omega Alpha. He completed a medical residency at New York Hospital-Cornell Medical Center in Manhattan before returning to Hopkins for his cardiology fellowship. During his tenure as a Robert Wood Johnson Clinical Scholar at Hopkins, he received an MA degree from the Institute of the History of Medicine. He chaired the Cardiology Department at Marshfield Clinic in Wisconsin from 1981 to 1999 and joined the Mayo Clinic in 2000.
Corporate Sponsors
2022 (May 11-14) Louisville, KY Annual Meeting
Program
Wednesday, May 11 |
|
| 2:30 pm | Registration: Outside the Lewis Salon |
| 3:00 pm | Executive Committee Meeting (Lincoln Boardroom) |
| 5:30 pm | Opening Welcome Reception (Jefferson Atrium) |
Thursday, May 12 |
|
| 7:00 am | Registration: Outside the Lewis Salon |
| 7:00 am | Complimentary Breakfast (Breakfast area) |
Session A |
|
| 8:15 am | Welcome: Joshua Bornhorst (President of the Association) Greetings: Eyas Hattab (Chair, Dept. of Path & Lab Med) Welcome: Roland Valdes, Jr., Program Chair |
| 8:30 am | [1] Abraham J. Gitlitz Memorial Lecture: Development of a Broad-Spectrum Antiviral-based Intranasal Spray as a Pandemic Preparedness Strategy. Kenneth E. Palmer, (Louisville, KY) |
| 9:15 am | [2] Acetylation Pharmacogenomics: Paradigm for Informed Individual Risk Assessment Following Exposure to Environmental Carcinogens. David Hien, (Louisville, KY) |
| 10:00 am | Coffee Break (Embassy Foyer) |
| 10:30 am | [3] Rolling with the Punches: A Biosafety Program at a Research University Addresses COVID-19. Allen Helm, (Chicago, IL) |
| 11:00 am | [4] An interdisciplinary Post-Operative Personalized Pain Management Clinical Trial. Saeed Jortani, (Louisville, KY) |
| 11:30 am | Adjournment for Lunch |
Session C |
|
| 1:00 pm | [6] Claude P. Brown Memorial Lecture: The Many Roads to Steatohepatitis and Its Treatment. Craig McClain, (Louisville, KY) |
| 1:45 pm | [7] Bioactive Lipid Metabolites: Novel Therapeutic Targets and Potential Treatment Strategies in Alcohol-Associated Liver Disease. Irina A. Kirpich, (Louisville, KY) |
| 2:15 pm | [8] Hepatic Protein and Phosphoprotein Signatures of Alcohol-Associated Hepatitis. Josiah E. Hardesty, (Louisville, KY) |
| 2:30 pm | [9] Soluble Epoxide Hydrolase Inhibition in Alcohol-Associated Liver Disease: Liver-Specific Drug Delivery. Jeff B. Warner, (Louisville, KY) |
| 2:45 pm | [10] COVID-19 and Early Post-Primary TB: Commonalities of Pathobiology Pneumonitis and Therapies. Robert Brown, (Houston, TX) |
| 3:00 pm | Refreshments (Embassy Foyer) |
Session D |
|
| 3:30 pm | [11] Plasma ctDNA for Monitoring Response to Immune Check Point Inhibitors. Mark W. Linder, (Louisville, KY) |
| 4:00 pm | [12] Quantitative Methods of Monitoring Circulating Tumor DNA. Evan Alexander, (Louisville, KY) |
| 4:30 pm | [13] Value of Next Generation Sequencing in Myeloid Neoplasia. Mustafa Al Kawaaz, (Louisville, KY) |
| 5:00 pm | [14] Forecasting Clinical Behavior and Therapeutic Response of Breast Carcinoma using Gene Expression. James Wittliff, (Louisville, KY) |
| 5:30 pm | Adjournment |
| 5:30 pm | Welcome Reception (King Lewis Atrium) |
| 7:30 pm | Musicale Rehearsal (William Salon) |
| 7:30 pm | Young Fellows Section social event & CCFP event led by Chris Crutchfield. (TBA). Open to all registrants ≤ age 45 and guests. |
Friday, 13 May |
|
| 7:00 am | Registration: Outside the Lewis Salon |
| 7:00 am | Complimentary Breakfast (Breakfast area) |
Session E |
|
| 8:15 pm | [15] Imaging Mass Spectrometry: Applications in Biomedical Research and Clinical Diagnosis. Yusheng Zhu, (Hershey, PA |
| 8:35 am | [16] Immune Landscape in Sentinel Lymph Nodes from Melanoma Patients by Single-Cell Mass Cytometry (CyTOF) Analysis. Kavitha Yaddanapudi, (Louisville, KY) |
| 8:55 am | [17] Application of MassARRAY System in Molecular Diagnostics - Pharmacogenomics and Oncology. Shuko Harada and Alexander Mackinnon (Birmingham, AL) |
| 9:20 am | [18] Alzheimer’s Disease CSF Biomarkers in Clinical Practice: Analytical and Clinical Considerations. Alicia Algeciras-Schimnich, (Rochester, MN) |
| 9:40 am | Coffee Break (Embassy Foyer) |
| 10:00 am | [19] Evaluation of SARS-C0V-2 Viral RNA Detection, Using Massarray, RT-qPCR and UltraFast RT-PCR Assays. Bene Ekine-Afolabi, (Sandwich, Kent, UK) |
| 10:20 am | [20] From the Microbiology Lab to the Operating Room: Advanced Development of the MasSpec Pen for Broad Clinical Use. Livia Eberlin, Houston, TX |
| 10:40 am | Adjournment |
Tour: Churchill Downs Museum |
|
| 11:00 am | Bus departs from hotel for special tour (tickets required) |
| 11:30 am | Afternoon tour - Churchill Downs, includes museum movie, lunch, and horse racing |
| 4:30 pm | Bus returns to Hotel |
Saturday, 14 May |
|
| 6:30 am | Run for the Lilies (meet in hotel lobby) |
| 7:00 am | Registration: Outside the Lewis Salon |
| 7:00 am | Complimentary Breakfast (Breakfast area) |
Session F |
|
| 8:30 am | [21] Triggered MRM for Urine Drug Testing: Finding What You Aren’t Looking For. Joshua Hayden, (Louisville, KY) |
| 8:45 am | [22] Advances in the Assessment of Orexin-A (hypocretin-1) Deficiency in the Diagnosis of Type 1 Narcolepsy. Joshua Bornhorst, (Rochester, MN) |
| 9:00 am | [23] Zika Outbreak in Dominican Republic 2016: A Review. Frederick Kiechle, (Boca Raton, FL) |
| 9:15 am | [24] Rapidly Evolving and Fatal Military Tuberculosis and COVID-19 Infection in an Infant. Anindita Ghosh (Houston, TX) |
| 9:30 am | [25] A Postulated Cross Talk between Insulin Growth Factor Binding Protein 3 (IGFBP-3) and IGFBP-7 May Suggest a Critical Role in Carcinogenesis. Fan Shen, (Edmonton, AB, CA), paper to be presented by Consolato Sergi (Ottawa, ON, Canada) |
| 9:45 am | Refreshments (Embassy Foyer) |
| 10:00 am | [26] Measure Directly, Treat Efficiently. Critical Bleeding Management at the Speed of Sound. Oksana Volod, (Los Angeles, CA) |
| 10:30 am | [27] Managing the Challenges of Running a Transfusion Service During the COVID-19 Pandemic. Claire Meena-Leist, (Louisville, KY) |
| 10:50 am | [28] Cells, Wells, & Spells: the Evolution of HLA Testing Methods. Tiffany Bratton, (Louisville, KY) |
| 11:10 am | [29] The CNS-Penetrating Taxane Drug TPI 287 Potentiates the Antiglioma Activity of the AURKA Inhibitor Alisertib in vivo. Müge Sak, (Louisville, KY) |
| 11:30 am | [30] SARS-CoV-2 Antibody Testing in the Post-Vaccine Era: Comparing Assays for Standardization. Sarrah Lahorewala, (Houston, TX) |
| 11:45 am | Adjournment |
| 12:00 pm | Lunch and ACS Business Meeting (Lewis Salon) Note: all attendees are invited to attend the ACS Business Meeting, although only Fellows of the Association may vote. |
| 1:20 pm | Adjournment |
Session G |
|
| 8:30 am | [31] How to be a Better Surgical Pathology Consultant. Neda Zarrin-Khameh, (Houston, TX) |
| 9:00 am | [32] The Diagnostic Role of Fusion-Gene Analysis in Ambiguous Bone and Soft Tissue Neoplasms. Haider Mejbel, (Birmingham, AL) |
| 9:25 am | [33] Distinct Lesions of Host Defense and Bacterial Offense in Tuberculosis. Robert Hunter, (Houston, TX) |
| 9:50 am | efreshments (Embassy Foyer) |
| 10:10 am | [34] Agonal-Stress Vesicles in Critically Ill Children Confused with Microvesicular Steatosis. John Hicks, (Houston, TX) |
| 10:35 am | [35] Transmission Electron Microscopy (TEM): A Tool Often Underused for Pediatric Small Round Blue Cell Tumors Opening New Venues for Single-Cell Technologies. Consolato Sergi, (Ottawa, ON, Canada) |
| 11:00 am | [36] Chondroid Chordoma Presenting as Oropharyngeal Mass in Pediatrics. John Hicks, (Houston, TX) |
| 11:25 am | [37] Deciduosis Adjacent to an Ileouterine Fistula in the Setting of Crohn’s Disease: Case Report and Literature Review. Lance Van Truong (Providence, RI) |
| 11:45 am | Adjournment |
Session H |
|
| 1:30 pm | [38] Modern Implementation of Digital Pathology with Artificial Intelligence in an Academic Medical Center. Dibson Dibe-Gondim, (Louisville, KY) |
| 2:00 pm | [39] Establishing a Hospital AI Committee: Enhancing Precision Medicine. Andrew A. Borkowski, (Tampa, FL) |
| 2:30 pm | [40] Artificial Intelligence in Radiology: Hype, Hope, or Hysteria. Narayan A Viswanadhan, (VA, Tampa, FL) |
| 3:00 pm | [41] Data Literacy in Healthcare: A Vital Component of Precision Medicine. Joyce J. Ou, (Providence, RI) |
| 3:30 pm | Refreshments (Embassy Foyer) |
| 3:50 pm | [42] Digital Health Applications and Key Characteristics Related to At-Home Testing Outcomes. Lee Springer (Boston, MA) |
| 4:20 pm | [43] Validation of Artificial Intelligence-Based System for Prostate Cancer Detection and Grading. Taryme Lopez Diaz, (Louisville, KY) |
| 4:45 pm | Adjournment |
Speaker Profiles
Abraham J Gitlitz Memorial Lecture | |
 |
“Drug Development in Academia During a Pandemic” Kenneth E. Palmer, PhD
Dr. Palmer was trained in molecular virology and biotechnology, first at the University of Cape Town, and then at Cornell University. His research program is focused on developing broad-spectrum antivirals for prevention and treatment of emerging and re-emerging viral infections. He started his career in the biotechnology industry, returning to academia at the University of Louisville in 2006 to grow a translational research program. He is a Professor of Pharmacology and Toxicology and Helmsley Endowed Chair in Plant-based Pharmaceutical Research in the University of Louisville School of Medicine. He is also Director of the University of Louisville Center for Predictive Medicine for Biodefense and Emerging Infectious Diseases, where he oversees the scientific operations of the University of Louisville Regional Biocontainment Laboratory. |
Claude P Brown Memorial Lecture | |
 |
"The Many Roads to Steatohepatitis and Its Treatment" Craig James McClain, MD, FACG, FAASLN, FACN
Dr. McClain, is a widely recognized expert in liver injury/disease, nutrition, and cytokine research, as well as hepatic drug metabolism. His laboratory currently focuses on nutrition and the gut:liver axis, especially as it relates to alcohol-associated liver disease and environmental liver disease. He has had continuous federal funding as PI for his research since 1977. Dr. McClain is a Past President of the American College of Nutrition, has served on several NIH and VA Study Sections and has published over 460 peer-reviewed articles and 110 book chapters/reviews. He has mentored over 125 Residents and Fellows including over 30 junior faculty members with K-type career development awards. Dr. McClain is currently leading the effort to develop ACG guidelines for nutrition in liver disease. |
Thursday Luncheon Speaker | |
 |
“Recent Advances in Artificial Heart Technology & Applications” Mark S. Slaughter, MD, FABS, FABTS
Dr. Slaughter is a clinician-scientist whose broad research focus is to understand the mechanisms of cardiac dysfunction and pathological remodeling in heart failure. He also has a particular interest in device-based therapy for cardiac disease, including mechanical circulatory support (MCS) devices, ventricular assist devices (VAD), and total artificial hearts (TAH). He is the Editor-in-Chief of the ASAIO Journal. In August, 2021, Dr. Slaughter and the cardiothoracic surgical team at UofL Health – Jewish Hospital implanted the Aeson® bioprosthetic total artificial heart into the first female patient in the world. The new device is intended as a bridge to a heart organ transplant, which is part of an Early Feasibility Study (EFS) sponsored by CARMAT, a French medical device company. |
Other Confirmed Speakers | |
 |
"Implementing digital pathology and AI in an Academic Health System" Dibson Dibe-Gondim, MD
Dr. Gondim has 12 peer-reviewed publications and is the winner of the 2019 Surgical Pathology Award for a poster that demonstrated, for the first time, an artificial intelligence model that can correctly classify the majority of the most common types of kidney neoplasms, presented at the 108th Annual Meeting of the United States and Canadian Academy of Pathology. |
| |
 |
“Application of circulating tumor DNA for monitoring response to Immune Check Point Inhibitors” Mark W. Linder, Ph.D., DABCC
Dr. Linder’s specialty is Clinical Chemistry and Toxicology. He has numerous publications and has developed the discipline of pharmacogenetics and its application to guide therapeutics. His research emphasis is now focused on circulating DNA analysis and applications to oncology.
|
| |
 |
“Measure Directly, Treat Efficiently. Critical Bleeding Management at the Speed of Sound” Oksana Volod M.D.
Dr. Volod earned her MD degree from Uzhgorod State University, Ukraine and completed postgraduate fellowship in hematopathology and coagulation and residency at Cedars Sinai, Los Angeles. She served on the Hemostasis and Thrombosis Committee of the College of American Pathologists (2015-2020) and also serves on the Pharmacy and Therapeutic Committee at CS and the Membership Committee of the International Society of the Hemostasis and Thrombosis (ISTH). She is an author of over 30 scientific publications and book chapters and an invited speaker at numerous regional, national, and international conferences.
|
| |
 |
“Acetylation pharmacogenomics: Paradigm for informed individual risk assessment following exposure to environmental carcinogens”, David W. Hein, Ph.D.
Dr. Hein serves as Peter K. Knoefel Endowed Chair of Pharmacology, Professor and Chairman of the Department of Pharmacology & Toxicology, and Distinguished University Scholar at the University of Louisville. His research program includes studies of the molecular epidemiology of cancer susceptibility, pharmacogenetics, genomics, personalized medicine, and functional genomics. In molecular epidemiology his work identifies individuals genetically susceptible to the development of cancer and other diseases from environmental and occupational chemicals in order to focus treatment and prevention public health strategies on those at greatest risk. The research in pharmacogenetics/ genomics and personalized/precision medicine improves our understanding of the genetic causes for drug failure and/or drug toxicity in order to optimize clinical drug therapy for each individual patient.
|
| |
 |
“Value of Next Generation Sequencing in Myeloid Neoplasia”, Mustafa Al-Kawaaz, MD
Dr. Al-Kawaaz received his M.D., from the Weill Cornell Medical College in Qatar in 2013. He completed his residency in Anatomic and Clinical Pathology and Fellowship in Hematopathology at Weill Cornell Medicine/New York Presbyterian Hospital in 2017. He completed a second fellowship in Molecular Genetic Pathology at the University of Chicago in 2018. Dr. Al-Kawaaz is triple board certified in Anatomic and Clinical Pathology and Hematopathology and is board eligible for Molecular Genetic Pathology. His research is focused on genomic alterations and clinicopathologic correlation in hematolymphoid malignancy with emphasis on large B cell lymphoma, chronic T cell neoplasms and myeloid neoplasms.
|
Corporate Sponsors
2021 (Nov. 4) Virtual Symposium: Diagnostic Management Teams: What They Are and How to Organize Them
Program
Thursday, November 4, 12:00 noon Central Time
| 12:00 | Welcome, Joshua Bornhorst, PhD, ACS President, Symposium Moderator |
| 12:05 | Michael Laposata, MD, PhD, “The Diagnostic Management Team: How it Works and What it Does.” Note – each talk includes a 10 minute Q&A |
| 12:35 | Michael Laposata, MD, PhD, “The Implementation of a COVID-19 Specific Diagnostic Management Team with Clinical and Financial Impacts.” |
| 1:05 | Break |
| 1:15 | Christopher Zahner, MD, “The Coagulation Diagnostic Management Team (DMT)’s Impact on Patient Care” |
| 1:45 | Peter McCaffery, MD, “Future of the Diagnostic Management Team: A Collaboration of Industry and Academia in a Global Network.” |
| 2:15 | Break |
| 2:25 | Eddie Salazar, PhD, MLS(ASCP)cm, “A New Curriculum to Train Doctoral Level Clinical Laboratory Scientists to Optimize Consultation by Laboratory Directors.” |
| 2:55 | Christopher Zahner, MD, “The Participation of the Doctoral Level Clinical Scientist (PhD or DCLS) in the Diagnostic Management Team Service.” |
| 3:25 | Break |
| 3:35 | General Discussion – asking the tough questions. Dr. Laposata and the speakers answer questions from the audience. |
| 4:00 | Program concludes |
Speaker Profiles
 |
Michael Laposata, M.D., Ph.D.
Dr. Michael Laposata is the Professor and Chair of the Department of Pathology at the University of Texas Medical Branch-Galveston and Director of the MD PhD Program at the university. He received his MD and PhD from Johns Hopkins University School of Medicine and completed a postdoctoral research fellowship and residency in Laboratory Medicine (Clinical Pathology) at Washington University School of Medicine in St. Louis. He took his first faculty position at the University of Pennsylvania School of Medicine in Philadelphia in 1985, where he was an Assistant Professor and Director of the hospital's Coagulation Laboratory. In 1989, he became Director of Clinical Laboratories at the Massachusetts General Hospital and was appointed to the faculty in the Department of Pathology at Harvard Medical School, where he became a tenured full Professor of Pathology. Dr. Laposata joined Vanderbilt University School of Medicine in 2008 where he was the Edward and Nancy Fody Professor of Pathology and Medicine. Additionally, he was Pathologist-in-Chief at Vanderbilt University Hospital and Director of Clinical Laboratories. His basic research program has focused on fatty acids and their metabolites. Dr. Laposata's clinical expertise, for both patient care and clinical research, is in blood coagulation, with a special expertise in diagnostic errors. He has authored more than 170 peer-reviewed publications in basic and clinical research. His work on diagnostic errors earned him an appointment to the 21-member panel of the National Academy of Medicine which issued the 2015 report on Improving Diagnosis in Healthcare. Dr. Laposata is the recipient of 14 major teaching prizes at Harvard, the Massachusetts General Hospital, and the University of Pennsylvania School of Medicine. His recognitions include the 1989 Lindback Award, a teaching prize with competition across the entire University of Pennsylvania system; the 1998 A. Clifford Barger mentorship award from Harvard Medical School; election to the Harvard Academy of Scholars in 2002, and to the Vanderbilt University School of Medicine Academy for Excellence in Teaching in 2009; and the highest award - by vote of the graduating class - for teaching in years 1 and 2 at Harvard Medical School in 1999, 2000, and 2005. His textbook, in its third edition, Laposata’s Laboratory Medicine, has been translated into multiple languages. It is used globally by those learning laboratory medicine and those using the clinical laboratory. In a peer nominated survey performed by The Pathologist, a journal reporting on the practice of pathology, the November 2015 issue identified Dr. Laposata as the most influential pathologist in the United States, and the third most influential pathologist in the world. |
 |
Christopher Zahner
Dr. Christopher Zahner is the Clinical Pathology Division Director, Diagnostic Management Team coordinator, the medical director of the Coagulation laboratory, and Point-of-Care testing in the Department of Pathology at the University of Texas Medical Branch. Dr. Zahner’s clinical research is focused on diagnostic error reduction using the diagnostic management team and related mobile app development. His research is focused on medical devices and resulted in hardware development, with patents in laboratory automation, sample processing, microbial growth, and hardware in sample tracking and hand hygiene. Prior to medicine, Dr. Zahner was a mechanical engineer for the National Aeronautics and Space Administration (NASA) for the International Space Station (ISS) specializing in Environmental Control and Life Support systems. |
 |
Peter McCaffrey
Dr. Peter McCaffrey is director of the Division of Pathology Informatics and Artificial Intelligence in the Department of Pathology of the University of Texas Medical Branch. He is a graduate of Johns Hopkins School of Medicine, and completed a residency in clinical pathology/laboratory medicine at the Massachusetts General Hospital. He then was accepted into a prestigious 1 year fellowship in medical informatics in the Texas Medical Center in Houston. At UTMB, Dr. McCaffrey also serves as assistant director of the clinical chemistry laboratory. He leads multiple multi-institutional groups focused on optimization of personalized interpretations as used in the diagnostic management team format. His research is focused on creation of expert diagnostic teams that can communicate globally with care providers in need of recommendations for test selection and interpretation of test results. Dr. McCaffrey is the architect of the information system which allowed UTMB to provide personalized interpretations about infectious status and antibody significance for all patients being tested for SARS-CoV-2. |
 |
J. Eddie Salazar, PhD, MLS(ASCP)cm
J. Eddie Salazar, PhD, MLS(ASCP)cm is Chair of the Department of Clinical Laboratory Science in the School of Health Professions at the University of Texas Medical Branch (UTMB) in Galveston, Texas. Dr. Salazar also holds a faculty appointment in the Department of Pathology at UTMB and serves as program director for the Doctorate in Clinical Laboratory Sciences (DCLS) program. Dr. Salazar also chairs the American Society for Clinical Laboratory Sciences DCLS national committee. Dr. Salazar received a Bachelor of Science in Clinical Laboratory Science from the University of Texas Medical Branch, a Master of Science in Instructional Technology from the University of Houston Clear Lake, and a Doctorate in Philosophy from Texas Tech University. His research interests include advanced practice in clinical laboratory sciences, reduction in diagnostic error, interprofessional education, educational technology, and curriculum development. |
Speaker Abstracts
Michael Laposata, MD, PhD, “The Diagnostic Management Team: How it Works and What it Does.”
This presentation will focus on the function of a diagnostic management team from the point at which the case is identified until the recommendations for test selection and correct interpretation of results are delivered into the medical chart. There is variability in how the diagnostic management team (DMT) operates in different clinical areas because of the different needs for information in different medical areas, such as coagulation vs. toxicology. For all diagnostic management teams, there is a role for the trainee to create tentative recommendations and interpretations for modification before final entry by the laboratory director into the medical record. The DMT is an opportunity to educate trainees on a case-by-case basis by the clinical laboratory scientist who leads diagnostic management team rounds, whose clinical expertise also continuously grows. The presentation will also note the clinical impacts of shortened length of stay and improved test utilization from the DMT.
Michael Laposata, MD, PhD, “The Implementation of a COVID-19 Specific Diagnostic Management Team with Clinical and Financial Impacts.”
There have been many diagnostic uncertainties related to testing for infection and for antibody response to the SARS-CoV-2 virus. The variability between the many PCR tests in sensitivity is substantial, at least a thousand fold from the most sensitive to the least sensitive. In addition, the false negatives associated with the inability to swab an infected area in the respiratory tract, and thereby obtaining a false negative result for patients who are truly infected, has been confusing to many healthcare providers. The clinical implications of positive tests for IgM antibodies and IgG antibodies were confounded by the different methodologies used to identify the antibodies and for some tests, quantify the antibodies. Many lateral flow tests to assess antibodies, in particular, showed significant cross-reactivity with antibodies to several different viruses. To address these difficulties, a diagnostic management team (DMT) focused on the interpretation of tests for each individual patient receiving Covid related tests was initiated. The major challenge was the large number of samples, and this forced an invention in which the EPIC medical database was “taught” to select 1 of more than 150 written interpretations written by the laboratory director and suggest it as the correct interpretation of the test results. It has been a substantial effort to create and then update on a near weekly basis the interpretive comments presented to EPIC as a possible interpretation as more information is learned and reported in the medical literature. The clinical impact of this patient specific expert driven report, which is available to both doctors and the patients who were tested, has been substantial. It has also possible to bill for these reports. The revenue generation from this single Covid DMT in our institution exceeded the revenue generated from surgical pathology.
Christopher Zahner, MD, “Length of Stay Reduction Using a Coagulation Diagnostic Management Team.”
The question posed in this presentation is whether the coagulation diagnostic management team (DMT) at the University of Texas Medical Branch has resulted in a shorter length of stay for patients with bleeding or clotting disorders. A previous study at Vanderbilt indicated that both pulmonary embolism and hemorrhagic stroke patients, specifically, experienced a major reduction in length of stay and lower expense per case upon the introduction of a coagulation diagnostic management team in July, 2010. The current study, unlike the previous one, involves the analysis of large amounts of data over several years. The same benefit was recognized, but this investigation indicated that the presence of a report with recommendations for testing and interpretation of test results was not likely to be the major reason for the observed improvement in clinical outcomes. The data show that the creation of a diagnostic management team within an institution leads to markedly enhanced, clinically meaningful communications between laboratory experts and patient facing providers. This is analogous to the longstanding valued communication between radiologists and clinicians about selection of an imaging study and the interpretation of the findings. It has been shown that a query to the clinical laboratory today too often leads to a person who performed the test but has no knowledge of the clinical case. The actual presence of a diagnostic management team appears to create a link for consultation about laboratory tests.
Peter McCaffery, MD, “Future of the Diagnostic Management Team: A Collaboration of Industry and Academia in a Global Network.”
From the experience of the diagnostic management team for SARS-CoV-2 related results at the University of Texas Medical Branch, it was clear that the challenge of creating "smart" programs within EPIC to select one of many prewritten comments, as a possible interpretation for entry into the medical record, required partners in industry for technological developments. Identifying experts within academia who can provide a series of recommendations for test selection and result interpretation is a major but manageable obstacle. However, the need for a smart system that can with very high likelihood suggest to a laboratory expert what the correct narrative report should be is a challenge of the highest magnitude. In this presentation, it will be described how a clinical laboratory expert focused on the generation of hundreds of possible comments related to more than 150 sets of laboratory test results, while the industry partner assumed responsibility for creation of the smart system which suggested the correct one for each specific set of results. It is expected that the product that results from the collaboration of academic experts and industry will make it possible to generate diagnostic management teams across the world who can assist health care providers as the test menu becomes increasingly large and more costly. This presentation will describe a specific academia and industry collaboration that is rapidly evolving.
Eddie Salazar, PhD, MLS(ASCP)cm, “A New Curriculum to Train Doctoral Level Clinical Laboratory Scientists to Optimize Consultation by Laboratory Directors.”
It has long been recognized that the clinical laboratory sciences graduate has not had a doctoral level opportunity within the field since its creation. At the same time, the complexity of laboratory testing and the cost associated with the misuse of tests both continue to grow. At the University of Texas Medical Branch, a curriculum was developed in 2016 to train clinical laboratory scientists at the doctoral level. There is a high degree of focus for these graduates to serve as intermediate care providers for clinical laboratory activities, like pathology assistants in anatomic pathology. This presentation will discuss the development of the curriculum, with a focus on the clinical training and development of diagnostic skills of the doctoral students. The students are educated along with medical students at DMT rounds. They are responsible for generating recommendations for test selection and correct interpretation of complex test results, just as the residents in pathology, in at least 6 different diagnostic management teams. The service roles of now 3 full classes of graduates, along with the individual thesis work of each, will be included in the presentation.
Christopher Zahner, MD, “The Participation of the Doctoral Scientist in Clinical Laboratory Science (DCLS) in the Diagnostic Management Team Service.”
It is impossible for most doctoral level laboratory directors to create and manage a diagnostic management team (DMT) without the support of an individual who queries the medical record and reviews all the laboratory test results to create a preliminary set of recommendations for testing and interpretation of the test results. Most pathology residency programs cannot provide a person to perform this duty for all the rotations which benefit from a patient specific, expert driven DMT report. As a result, there is abundant opportunity for graduates of the doctorate in clinical laboratory sciences (DCLS) program to serve in this role, especially because they could be "permanently" associated with a specific diagnostic management team rather than rotating from one to another as residents do. The impact of the DCLS graduate in the clinical laboratory may be larger in smaller institutions, where there is often less institutional expertise about test selection and result interpretation. This presentation focuses on the evolving role of DCLS graduate in connecting healthcare providers in a meaningful way to experts within the clinical laboratory.
orporate Sponsors
The Association of Clinical Scientists greatly appreciates the sponsorship of the following company for this virtual symposium on Diagnostic Management Teams.:

2021 (May 13-14) Virtual Annual Meeting
Program
Final Program (all times CDT)
Thursday, May 13 Theme: Emerging Technologies in Clinical Laboratory Medicine
| 1:00 pm | Claude P. Brown Memorial Lecture Faisal Khan, PhD, University of Calgary, “Towards Improved Outcomes of Hematological Malignancies: Three Approaches of Precision Medicine.” |
| 1:40 pm | Q&A |
| 1:50 pm | David Murray, MD, PhD, Mayo Clinic, “The journey to replace immunofixation with mass spectroscopy for plasma cell disorders.” |
| 2:30 pm | Q&A |
| 2:40 pm | James Broach, PhD, Penn State Cancer Institute, “Comprehensive identification of structural variants, the dark matter of cancer genomics.” |
| 3:20 pm | Q&A |
| 3:30 pm | Presentation of Young Clinical Scientist Award by Myra Wilkerson, MD, Awards Chair, to Amanda Haynes, DO. |
| 3:40 pm | George G Chen, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, NT, Hong Kong, Estrogen receptor alpha-mediated autophagy promotes the survival of papillary thyroid cancer via enhancing the levels of ERK1/2 and reactive oxygen species but inhibiting NRF2. |
| 3:55 pm | Deblina Mukherjee, St. George’s University School of Medicine, St. George’s, Grenada, St. Joseph’s Children’s Hospital, Paterson, NJ, and St. Joseph’s University Medical Center, Paterson, NJ, Regression of COVID-19 ICFR to CFR for the United States and Europe. |
| 4:05 pm | Q&A |
| 4:10 pm | Erica Fatica, Mayo Clinic, Rochester, Clinical laboratory testing for macro-aspartate aminotransferase (macroAST): 8 years of experience. |
| 4:20 pm | Q&A |
| 4:25 pm | Norah Alghamdi, University of Louisville, Louisville, KY, A proposed novel biomarker for post-traumatic stress disorder (PTSD). |
| 4:35 pm | Q&A |
| 4:40 pm | Devereaux Sellers, Department of Pathology, The MetroHealth System, Cleveland, OH, and Department of Pathology, Case Western Reserve University School of Medicine, Cleveland, OH, Stark disparities between multiplex bead-based technology vs. immunofluorescence assay. |
| 4:50 pm | Q&A |
| 4:55 pm | Brenda Mai, University of Texas Health Science Center, Houston, TX, A Case Report of Fetal Thrombotic Vasculopathy in a COVID Placenta. |
| 5:05 pm | Q&A |
| 5:10 pm | Prasenjit Mitra, All India Institute of Medical Sciences, Jodhpur, India, Molecular aspects of lead toxicity. |
| 5:20 pm | Q&A |
| 5:25 pm | Taru Goyal, All India Institute of Medical Sciences, Jodhpur, India, Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers. |
| 5:35 pm | Q&A |
| 5:40 pm | Program concludes |
Friday, May 14 Theme: COVID-19 Surveillance in Public Health
| 1:00 pm | Abraham J. Gitlitz Memorial Lecture Maria Elena Bottazzi, PhD, Baylor College of Medicine, “International Efforts in Combatting COVID19: Behind the Scenes of How to Develop a COVID-19 Vaccine Suitable for Global Access.” |
| 1:50 pm | Q&A |
| 2:00 pm | Presentation of FW Sunderman, Jr. Diploma of Honor by Myra Wilkerson, MD, Awards Chair, to Robert W. Hardy, PhD. |
| 2:10 pm | Michael Pentella, PhD, D(ABMM), University of Iowa, College of Public Health, “The Collaboration of Clinical and Public Health Laboratories to Provide COVID Testing Services.” |
| 2:50 pm | Q&A |
| 3:00 pm | Presentation of Clinical Scientist of the Year Award by Myra Wilkerson, MD, Awards Chair, to Keri J. Donaldson, MD, MSCE. |
| 3:10 pm | Jill E. Weatherhead MD, PhD, CTropMed, Baylor College of Medicine, “Impact of the COVID-19 Pandemic on Vulnerable Immigrant Communities in the United States.” |
| 3:50 pm | Q&A |
| 4:00 pm | ACS 2021 Annual Business Meeting, Keri J. Donaldson, MD, MSCE, presiding. |
| 5:00 pm (approx.) | Program concludes |
Speaker Profiles
Thursday, May 13: Session Theme: “Emerging Technologies in Clinical Laboratory Medicine” |
|
 |
Faisal M. Khan, PhD, University of Calgary, Claude P. Brown Memorial Lecture “Towards Improved Outcomes of Hematological Malignancies: Three Approaches of Precision Medicine.” Dr. Faisal M. Khan is an Associate Professor at the University of Calgary. In his clinical role, Dr. Khan works as the Clinical Director of Hematology Translational Lab, the Associate Clinical Director of Histocompatibility and Immunogenetic Lab (HIL) and as Scientific Lead of Molecular Pathology Program in Alberta Precision Labs. Dr. Khan obtained his PhD in Human Molecular Genetics in India in 2006. He completed his postdoctoral training and clinical fellowship at the University of Calgary. Dr. Khan is a certified Diplomate of American Board of Histocompatibility and Immunogenetics (ABHI). Dr. Khan has more than 21 years of experience in Transplant Immunology, Cancer Genomics and Histocompatibility and Immunogenetics. Based on his research, Dr. Khan has published 87 research articles in scientific journals like Science, Blood, and Blood Advances. His research has been recognized by several awards including American Society of Hematology (ASH) Achievement Awards in 2013, 2015 and 2018. |
 |
David Murray, MD, PhD, Mayo Clinic, “The Journey to Replace Immunofixation with Mass Spectroscopy for Plasma Cell Disorders.”
Dr. Murray is a physician scientist who oversees the clinical protein immunology laboratory at The Mayo Clinic, Rochester. Before attending medical school, he spent 10 years performing research related to macromolecules for Dow Corning and Eastman Chemical Company. He is also a board certified anatomical and clinical pathologist. His research goals center on the adoption of proteomics into the clinical lab. His work had resulted in over 60 peer reviewed articles, 38 patents and a novel mass spectroscopic proteomic assays adapted into the clinical laboratory. Dr. Murray is Consultant, Division of Clinical Biochemistry and Immunology, Department of Laboratory Medicine and Pathology and an Assistant Professor of Laboratory Medicine and Pathology. He holds a PhD in polymer chemistry from the University of Akron and an MD from East Tennessee State University. He completed a residency in anatomic and clinical pathology at the Mayo School of Graduate Medical Education in the Mayo Clinic College of Medicine. |
 |
James Broach, PhD, Penn State Cancer Institute, “Comprehensive identification of structural variants, the dark matter of cancer genomics.”
Dr. Broach is Distinguished Professor and Chair of the Department of Biochemistry and Molecular Biology at Penn State College of Medicine and Director of the Institute for Personalized Medicine. Dr. Broach was Professor of Molecular Biology at Princeton University from 1984-2012, where he served as Associate Director of the Lewis Sigler Institute for Integrative Genomics and Co-Director of the Center for Computational Biology. Dr. Broach has served as Chair of the Genomics, Computational Biology and Technology Study Section at NIH as well as chair of numerous special emphasis genomics panels. He was Co-Founder and Director of Research for Cadus Pharmaceuticals from 1992 to 2000. Dr. Broach is a Fellow of the American Academy of Microbiology and of the American Association for the Advancement of Science. Dr. Broach has published more than 175 articles in the area of molecular biology and genomics and holds a number of patents in drug discovery technologies. |
Friday, May 14: Session Theme: “COVID-19 Surveillance in Public Health” |
|
 |
Maria Elena Bottazzi, PhD, FASTMH, Baylor College of Medicine, Abraham J. Gitlitz Memorial Lecture, “International Efforts in Combatting COVID19: Behind the Scenes of How to Develop a COVID-19 Vaccine Suitable for Global Access.”
Dr. Bottazzi is Associate Dean of the National School of Tropical Medicine, Professor of Pediatrics and Co-director of Texas Children’s Center for Vaccine Development at Baylor College of Medicine in Houston, Texas. She is an internationally recognized tropical infectious disease vaccinologist and global health advocate with two decades pioneering and leading the advancement of a vaccine portfolio from discovery to clinical trials for diseases, such as coronavirus, hookworm, schistosomiasis, and Chagas, all neglected diseases that affect disproportionally the world’s poorest populations. She also has established innovative partnerships in Latin America, Middle East and South East Asia, making significant contributions to innovative educational/research programs and catalyze policies and disseminate science information to reach a diverse set of audiences. As a global thought-leader she has received national and international highly regarded awards, has more than 150 scientific papers and participated in more than 250 conferences worldwide. She is a Member of the National Academy of Science of Honduras and an Emerging Leader in Health and Medicine of the National Academy of Medicine in the US. Dr. Bottazzi currently serves as Co-chair of the Vaccines and Therapeutics Taskforce of the Lancet Commission on COVID-19. |
 |
Michael A. Pentella PhD, MS, SM(ASCP), CIC, DABMM, University of Iowa, College of Public Health, “The Collaboration of Clinical and Public Health Laboratories to Provide COVID Testing Services.”
Dr. Pentella is a Clinical Professor at the University of Iowa, College of Public Health and Director of the Iowa State Hygienic Laboratory. His experience spans over forty years in clinical microbiology and public health laboratories. He is certified as an American Board of Medical Microbiology Diplomate, a specialist in microbiology through the American Society for Clinical Pathology, and certified in infection control through the Association of Professionals in Infection Control. Dr. Pentella is a member of the Association of Public Health Laboratories (APHL) Antibiotic Resistance Lab Workgroup, the APHL Biosafety and Biosecurity Committee (chair), and the APHL Influenza Committee. He has made several contributions that have improved the practice of clinical microbiology. He has written over 50 articles and fifteen book chapters. |
 |
Kelly Oakeson PhD, Utah Public Health Laboratory, Salt Lake City, UT, “Surveillance of SARS-CoV-2 Variants.”
Dr. Oakeson, is the Utah Public Health Laboratory chief scientist for next-generation sequencing and bioinformatics. He received both his bachelor’s and Ph.D. from the University of Utah. He joined the Utah Public Health lab in 2016. Under his leadership, Utah PHL has become a leader in public health in the utilization of next-generation sequencing for disease surveillance and detection. Utah PHL is the CDC Mountain Region’s Bioinformatics regional resource. He is part of the APHL Infectious Disease and Food Safety Committee. |
 |
Jill E. Weatherhead, MD, PhD, CTropMed, Baylor College of Medicine, “Impact of the COVID-19 Pandemic on Vulnerable Immigrant Communities in the United States.”
Dr. Jill Weatherhead is an Assistant Professor of Pediatrics and Medicine in the Sections of Pediatric Tropical Medicine, Pediatric Infectious Diseases and Adult Infectious Diseases at Baylor College of Medicine (BCM). She obtained her MD from Michigan State University and her PhD from Baylor College of Medicine where she also completed her clinical residency and fellowship in combined adult and pediatric infectious diseases. Dr. Weatherhead serves as the Director of Medical Education at the National School of Tropical Medicine (NSTM) at BCM as well as the clinic director for the Adult and Pediatric Tropical Medicine Clinic. She provides clinical care within the Harris Country Health System which is a safety net system that services uninsured people living in Houston, TX. During the COVID pandemic she has called attention to the disproportionate effects COVID-19 has had on vulnerable communities in the US and the importance of vaccine rollout in hard-hit communities. |
Speaker Abstracts
Invited Speakers
Faisal M. Khan, PhD, University of Calgary
Towards Improved Outcomes in Hematologic Malignancies: Three Approaches of Precision Medicine
Prognosis of hematological malignancies like Acute Myeloid Leukemia (AML) and B cell NonHodgkin’s Lymphoma (NHL) is far from ideal, primarily due to frequent relapse and/or failure of treatment. Management of relapse is ineffective, whereas preemptive treatment of impending relapse is effective. However, existing approaches for early and reliable detection of impending relapse of malignancy are not successful. Building upon the research of several years, our team at University of Calgary is studying three synchronized approaches to identify most effective treatment strategy for AML/B-cell NHL and provide early and accurate prediction of leukemia relapse.
David Murray, MD, PhD, Mayo Clinic
The Journey to Replace Immunofixation with Mass Spectroscopy for Plasma Cell Disorders
This presentation will focus on the development, validation and implementation of a MALDI-TOF MS method as a replacement for traditional immunofixation electrophoreses for isotyping monoclonal proteins. The journey began in 2014 with studies involving high resolution LC-Q-TOF MS of tryptic peptides and intact immunoglobulin light chains with a goal of a serum based minimum residual disease detection in multiple myeloma patients. Subsequently, the method was adapted to a MALDI-TOF MS platform and coupled to IgG, IgA, IgM and kappa and lambda immunoenrichment termed Mass-Fix at Mayo Clinic. This was a key step which afforded the ideas of using the method in all aspects of multiple myeloma. Several studies involving both clinical and analytical performance of the assay demonstrated improvement over traditional electrophoretic analysis. Several patient cases will be presented to demonstrate these improvements which include increased specificity, improved sensitivity and the detection of M-proteins with light chain glysoylation. The detection of light chain glycosylation was found to be a risk factor for the development of plasma cell disorders. Several challenges and hurdles were experienced during the automation and implementation of the assay. Currently, our lab has performed more than 50,000 assays by the Mass-Fix method.
James Broach, PhD, Penn State Cancer Institute
Comprehensive Identification of Structural Variants, the Dark Matter of Cancer Genomics
Genomic analysis of tumors has stimulated major advances in cancer diagnosis, prognosis and treatment, shifting the focus from morphological and histochemical characterization to consideration of the landscape of driver mutations in the tumor. To date such consideration has focused on somatic mutations comprising single nucleotide changes or small insertions or deletions. We have recently applied optical genomic imaging (OGM) to a variety of human tumors and showed that OGM can detect structural variants (SVs), including deletions, insertions, duplications, inversions and translocations, that are not easily detectable using standard methods of whole genome analysis. Our studies of more than 100 cases of Acute Myeloid Leukemia indicated that OGM identified all the clinically relevant SVs and copy number variants reported by standard cytogenetic methods, such as cytological karyotyping, fluorescent in situ hybridization and microarrays. Importantly, OGM identified clinically relevant SVs in a number of cases that had been missed by the routine methods and refined the underlying genomic structure reported by traditional cytogenomic testing in many other cases. We also applied OGM to Human Papilloma Virus (HPV) associated head and neck cancers, predominantly oropharyngeal carcinomas. We found the virus had integrated into the host genome in two thirds of the tumors examined but resided solely extrachromosomally in the other third. Focal amplification of the virus and the genomics sequences surrounding it often occurred subsequent to integration. In all cases, viral integration correlated with pervasive genome-wide somatic alterations, including multiple insertions, deletions, translocations, inversions and point mutations. Few or no somatic structural variants were present in tumors with only episomal HPV. In sum, our studies have shown that OGM identifies numerous somatic mutations that current genomic analysis methods fail to reveal and this capability can improve diagnostic and prognostic efforts when applied to a variety of cancers.
Maria Elena Bottazzi, PhD, Texas Children’s Center, Baylor College of Medicine
International Efforts in Combatting COVID19: Behind the Scenes of How to Develop a COVID-19 Vaccine Suitable for Global Access.
For the last two decades, the National School of Tropical Medicine and its Center for Vaccine Development in Houston, Texas has operated with the mission to develop and test new low-cost and effective vaccines against emerging and neglected tropical diseases, build capacity for vaccine development locally and with foreign nations and guide and influence vaccine policy and advocacy. This approach relies on the need for international diplomacy, solidarity, and cooperation. This presentation will provide a behind the scenes vignette and an overview of the vaccine development process as well as a review of the coronavirus vaccine development landscape. Finally, it will highlight a case study of how a COVID-19 vaccine, suitable for global access, was developed and is currently advancing towards achieving emergency use authorization for distribution and access this summer.
Michael A. Pentella PhD, MS, SM(ASCP), CIC, DABMM, University of Iowa, College of Public Health
The Collaboration of Clinical and Public Health Laboratories to Provide COVID Testing Services.
The risk of an emerging pathogen evolving into a pandemic is always present but, fortunately, it is a very rare event. The experience of COVID-19 is unprecedented and has reinforced to us the importance of preparedness for the rare event to prevent the devastation that the pandemic can cause. In considering COVID-19, never before has laboratory testing played such a vital role nor been in such high demand. As in past pandemics, there are several phases from the occurrence of a few human infections through widespread human infection, to the post peak phase, and eventual post pandemic phase. These phases must be considered when determining the need for laboratory testing. During past emerging infections, public health and clinical laboratories have worked in unison for effective care of the patient and prevention of further cases. For SARS-CoV-2 to make testing available to everyone who needed to be tested has taken the collaboration of clinical and public health laboratories to provide life-saving testing services. This was most critical at the start of the COVID-19 pandemic when few tests were available. Later, in the post peak phase, public health laboratories are dependent on clinical laboratories for samples to perform sequencing needed to track emergence of variants. Building statewide laboratory networks is a key factor in emergency preparedness efforts to respond to all phases of the pandemic, as well as outbreaks and epidemics. Leadership from public health laboratories is essential to build and maintain the network. Clinical laboratories must recognize their role in the network. The ongoing collaboration of clinical and public health laboratories to form a network best serves the patients and the population.
Kelly Oakeson, PhD, Utah Public Health Laboratory
Surveillance of SARS-CoV-2 Variants.
With the COVID-19 pandemic continuing, the SARS-CoV-2 is spreading and replicating and, as expected, mutating, evolving, and adapting. These variants lead to the rise of new lineages of SARS-CoV-2 that are more transmissible, can be resistant to medical interventions, and cause more severe illness. These new lineages or variants of concern pose new challenges for public health laboratories as they race to increase the genomic sequence of SARS-CoV-2 to detect variants of concern. The Utah Public Health Laboratory has been sequencing SARS-CoV-2 since the Pandemic started and is taking on the challenges of detecting variants of concern, including the issues of developing and validating whole-genome sequencing for SARS-CoV-2.
After listening to the presentation, the audience will understand the role that public health laboratories serve in the genomic surveillance of SARS-CoV-2.
Submitted Abstracts
Deblina Mukherjee1, Michael Lamacchia1,2 and Vincent A. DeBari 1,3, 1St. George’s University School of Medicine, St. George’s, Grenada, 2St. Joseph’s Children’s Hospital, Paterson, NJ, and St. Joseph’s University Medical Center, Paterson, NJ, Regression of COVID-19 ICFR to CFR for the United States and Europe.
Of obvious interest in the study of an epidemic is the case fatality rate (CFR), defined as the number of deaths divided by the number of cases, expressed as a percent. However, the actual CFR can only be computed after an epidemic has run its course and the total number of deaths and cases can be accurately ascertained. We define a metric, the Interim Case Fatality Rate (ICFR) computed as the longitudinal CFR on a bi-weekly basis. Herein, we examine the ICFR over the period March 1, 2020 when COVID-19 first appeared in substantial numbers to Jan 15, 2021. The purpose of this study was to ascertain whether longitudinal changes in ICFR would predict the likely ultimate CFR of COVID-19. We used open public source databases and derived ICFR from point estimates of cases and deaths for geopolitical entities in four regions each of the United States and Europe. Early in the pandemic, calculated ICFR were plotted and frequently found to represent a variably modal pattern with peak ICFR exceeding 15% in some cases. However, the curves were found to decrease and regress to relatively constant ICFR values. We postulated that actual CFR could be estimated when no statistically significant differences in sequential measurements of ICFR for the final monthly (three measurements) period could be detected. This resulted in estimates of case-weighted CFR [mean (95% confidence interval)] ranging from 1.77% (0.59 to 2.95) for the USA to 2.31% (1.85 to 2.77). We conclude that this suggests that early estimates of the CFR may provide highly erroneous estimates but that the ICFR may regress to an estimate of the actual CFR.
Upon completion of this activity, the participant should be able to: (1) recognize the variability in the ICFR of different geopolitical entities during the Covid-19 pandemic; (2) observe the manner in which the ICFR regresses to a constant value; and (3) calculate the weighted CFR predicted by this model.
Erica Fatica, Paige Menk, Darci Block, and Nikola Baumann, Mayo Clinic, Rochester, MN, Clinical laboratory testing for macro-aspartate aminotransferase (macroAST): 8 years of experience.
Macro-aspartate aminotransferase (macroAST) is a high-molecular weight complex that consists of aspartate aminotransferase (AST) bound to immunoglobulins. The macro-complex causes elevations in measured serum AST activity. Although clinically benign, identification of macroAST is important as patients may undergo years of unnecessary diagnostic investigations before macroAST is identified. To our knowledge, we are the only reference laboratory that offers macroAST testing. The aim of this retrospective analysis was to evaluate the distribution of results obtained, % of positive samples, and patient demographics for macroAST testing during an 8-year period (2013-2021). The macroAST assay involves measuring AST activity in serum before (total) and after polyethylene glycol (PEG) precipitation (post-PEG). PEG precipitation was performed by incubating samples with 25% PEG solution at a 1:1 ratio followed by centrifugation at room temperature for 5 minutes. The percent of PEG-precipitated AST activity (%PPA) was calculated as [(total – post-PEG)/total] x 100. A %PPA of >80% is positive for macroAST based on initial validation studies using controls and gel filtration chromatography-confirmed macroAST samples. 300 macroAST tests were ordered for 291 unique patients (181F, 110M). Patient ages ranged from 1 month to 93 years old with a median of 35 years (IQR 12-56). There were 137/300 (45.7%) positive samples, of which 105 (76.6%) were from female patients and 32 (23.4%) were from males. The median(range) of total AST results was 75(15-1196) U/L for macroAST-negative samples and 253(56-954U/L) for macroAST-positive samples. There was a bimodal distribution of %PPA results with a mean±SD %PPA of 31.3%+13.9% for population 1 (negative) and 92.2%+4.8% for population 2 (positive). The results show that almost 50% of physician-ordered macroAST tests were positive with macroAST found more frequently in female patients.
Upon completion of this activity, participants will be able to: (1) Describe the molecular composition and analytical difficulty presented by macroAST; (2) Describe patient demographics and characteristics of patients negative for macroAST; and (3) Describe patient demographics and characteristics of patients positive for macroAST.
Norah Alghamdi and Roland Valdes, Jr., University of Louisville School of Medicine, Louisville, KY, A proposed novel biomarker for post-traumatic stress disorder (PTSD).
Our work aims to test the hypothesis that subjects who suffer from Post-Traumatic Stress Disorder (PTSD) have an inherent dysregulation of the corticotropin-axis involving the neuropeptide Urocortin3 (UCN3) and its receptor Corticotropin Releasing Factor Receptor2 (CRFR2). PTSD is a condition that develops after a set of traumatic stressors. UCN3 is a corticotropin-releasing factor (CRF)-related peptide which plays a role in restoring homeostasis in response to stress via activation its receptor, CRFR2, resulting in mediating/dampening stress sensitivity. The diagnosis of PTSD is currently based on mental disorder criteria which are complex, subjective, and require human judgment. No clinical laboratory test is currently available to aid in this diagnosis, thus having a rapid and inexpensive biomarker test for PTSD would have substantial clinical impact. We hypothesize that in PTSD UCN3 secretion is deficient, causing the inability to cope with stress. Testing our hypothesis requires a high-sensitivity assay able to measure UCN3 in the sub-picogram per milliliter (pg/mL) range. This level of sensitivity is achievable using a combination of high affinity aptamers and monoclonal antibodies. Aptamers are sequenced nucleotides that bind to their targets with high affinity and specificity making them ideal diagnostic reagents. Our focus is to develop a high-sensitivity assay required to measure samples from PTSD subjects available through the Department of Veterans Affairs PTSD Biorepository Brain Bank (VABBB).
Upon completion of this activity, participants should be able to: (1) describe the PTSD condition and the limitations in current approaches to its diagnosis; (2) discuss the rationale for targeting UCN34 as a biomarker for PTSD; and (3) describe the advantages of using aptamers in developing diagnostic tests.
Devereaux Sellers1,2, Taha Keskin1,2, Linlin Yang1,2, and Mahesheema Ali1,2, 1Department of Pathology, The MetroHealth System, Cleveland, OH, and 2 Department of Pathology, Case Western Reserve University School of Medicine, Cleveland, OH, Stark disparities between multiplex bead-based technology vs. immunofluorescence assay.
Objective: To retrospectively examine the outcome of anti-nuclear antibody (ANA) screen by comparing the performance of BioPlex 2200 and immunofluorescence assay (IFA)
Methods: We reviewed ANA performance (Feb 2020 to Jan 2021) on BioPlex 2200 ANA using multiplex florescent beads (antigens dsDNA, chromatin, SSA 60, SSA 52, SSB, Sm, SmRNP, RNP A, RNP 68, Scl-70, Jo-1, ribosomal P, and centromere B) and immunofluorescence assay (using HEp-2)
Results: Total number of cases tested on both multiplex flow and IFA platform were 133 (111 females and 22 males). The prevalence in our population divided by age groups 18 to 44 years (36%); 45 to 64 years (42%); 65 years or older, (22%) has reported lupus. The mean age of the lupus patients at diagnosis is clustering around 53 years. Out of 133 multiplex tests performed, 58 tests were negative and 75 were positive. 47% of the tests performed with a negative result (58 tests) on multiplex flow turned to positive on IFA assay. The breakdown of titers for these tests were: 30% (1:320); 30% (1:160); 15% (1:80); and 26% (1:20). 55% of the tests performed with a positive result (75 tests) on multiplex flow turned to negative on IFA assay. The breakdown of titers for these tests were: 12% (1:1280), 18% (1:320); 6% (1:640); 15% (1:160); 15% (1:40); and 35% (1:80). Upon scrutinizing further, data shows a significant disparity in the dsDNA (27%) and RNP antibodies (51%) of the multiplex positive tests turned to negative on IFA assay.
Conclusion: Our data suggests a disparity between the results obtained from both the platforms. The common notion of IFA being a gold standard is flawed therefore manufacturer’s need to invest in optimizing assays that are less prone to errors. Clinicians should interpret the test results in clinical context that includes history, assessment of signs & symptoms.
Upon completion of this activity, the participant will be able to (1) identify the gaps between multiplex bead-based technology and immunofluorescence assay; (2) compare the performance of multiplex bead-based technology and immunofluorescence assay; and (3) recommend education on the disconnect between a patient’s symptoms versus test results.
Brenda Mai, Mesk Alrais, Amanda Tchakarov, and Nina Tatevian, University of Texas Health Science Center, Houston, TX, A case report of fetal thrombotic vasculopathy in a COVID placenta.
The aims and scope of this presentation are to highlight an interesting case report of a third trimester pregnancy with symptomatic coronavirus disease 2019 (COVID-19) complicated by fetal thrombotic vasculopathy (FTV). COVID-19 has affected patients of all ages and demographics, not excluding pregnant women. The effects of COVID-19 on pregnant women are largely still unknown. Several adverse perinatal outcomes have been reported in COVID-19-positive pregnant women including pre-eclampsia, miscarriage, pre-term labor, and stillbirth. Histopathological examination of COVID-19 placentas can contribute significant data regarding maternal and fetal health and elucidate more findings in this novel disease. A 23-year old female with morbid obesity and scant antenatal care presented to the emergency department complaining of shortness of breath and fever; she was found to be positive for COVID-19. Grossly, her placenta showed no abnormalities. Histological examination of her placenta showed chronic lymphoplasmacytic deciduitis, villous fibrosis, loss of capillarization, extravasation of erythrocytes, chorangiosis, and thrombosis of upstream stem vessels, including large fetal vessels on the chorionic plate. These changes were deemed to be consistent with FTV. FTV is a condition where blood clots cause obstruction of both arteries and veins, causing downstream occlusion, decreasing placental oxygen flow, impairing nutritional exchange, and causing ischemic changes and infarctions in the placental villi. FTV can result in serious fetal sequelae such as miscarriage/stillbirth, fetal intrauterine growth restriction, infarcted organs, neonatal stroke, neonatal encephalopathy, and cerebral palsy. Grossly, thrombosis of chorionic vessels can result in pale and firm placental parenchyma. Microscopically, organizing thrombosis, endothelial cell destruction, avascular fibrinoid necrosis, hemorrhagic endovasculitis, stromal karyorrhexis, fibromuscular sclerosis, fibrosis, and septation are frequent features. In conclusion, this case of FTV in the placenta in a patient with COVID-19 is a significant finding as this can be critical to clinicians for the management of prenatal care for expecting mothers during this pandemic.
Upon completion of this activity, participants should be able to: (1) identify the gross macroscopic findings in fetal thrombotic vasculopathy (FTV); (2) describe the histopathologic features of FTV; and (3) explain the fetal sequelae of FTV.
George G Chen, Zhongqin Gong, Lingbin Xue, Jason YK Chan, C Andrew van Hasselt, Alexander C Vlantis, Michael CF Tong. The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, NT, Hong Kong, Estrogen receptor alpha-mediated autophagy promotes the survival of papillary thyroid cancer via enhancing the levels of ERK1/2 and reactive oxygen species but inhibiting NRF2.
An increasing number of publications have indicated that estrogen receptor alpha (ERa) contributes to the development and growth of papillary thyroid cancer (PTC). However, the mechanism responsible remains largely unknown. Autophagy, a catabolic process by which cells degrade their own components by targeting them for lysosomal degradation. In this study, we aimed to explore the connections between ERa and autophagy in PTC. Using human PTC tissues, cell lines and mouse tumor models, we demonstrated that ERa could induce autophagy in PTC and that the upregulation of ERK1/2 and reactive oxygen species (ROS) predated the occurrence of autophagy. We also found that the level of heme oxygenase-1 (HO-1) was increased in the ERa-mediated autophagy cells compared with the control. The inhibition of Keap1further enhanced the expression of HO-1 but limited the levels of ROS as well as the autophagy, sensitizing PTC cells to chemotherapeutic agents. On the other hand, the inhibition of NRF2 led to the downregulation of HO-1 and further increase the autophagy, resulting in the tumor cells less sensitive to the chemotherapies. In the mouse tumor model, tumors formed by PTC cells with ERa overexpression grew significantly larger, with enhanced autophagy. The application of methyl-piperidino-pyrazole (MPP), a selective ERa antagonist could markedly reduce the growth of the tumor with decreasing autophagy. Therefore, our results have confirmed that ERa-induced autophagy is a survival factor for PTC. Importantly, it appears that increase of HO-1 in ERa-induced autophagy is a compensatory or control mechanism of the tumor cells to control their growth. These data suggest that there are potential therapeutic targets to arrest the growth of PTC, including ERa, HO-1 and Keap1 and NRF2 (Supported by grants from the National Natural Science Foundation of China, No.81972493, the Research Grants Council of the Hong Kong SAR, GRF 14109716).
After completing this activity, the learner will be able to (1) appreciate how ERa contributes to growth of papillary thyroid cancer (PTC); (2) discuss the role of HO-1 as a potential target for treatment of PTC; and (3) discuss the role of NRF2 as potential target for treatment of PTC
Prasenjit Mitra, All India Institute of Medical Sciences, Jodhpur, India, Molecular aspects of Lead toxicity.
This session will mainly highlight molecular aspects of Lead toxicity. The novel molecular markers that are involved in lead toxicity will be discussed in details. The markers will be classified as genomic and epigenetic markers. Genomic markers would include the Single Nucleotide Polymorphisms (SNPs). Epigenetic markers would include DNA methylation, Histone modification and miRNAs. The latest molecular mechanism that are being identified would be enlightened. Lead toxicity is a big problem not only in developing countries like India but reports indicate it to be a grave issue even in developed countries like United States. In developed countries, children are more affected than adults, while in developing countries, both children and adults especially the occupationally exposed individuals are at high risk of developing lead toxicity. Earlier World Health Organization recommended a Blood Lead Level (BLL) of 5 µg/dl as a safe level. But the safety levels have changed and now no lead level is considered safe. Lead in children affects nervous system and gradually leads to IQ reduction along with other manifestations. In adults, it is a potent carcinogen. Research should identify novel biomarkers that may aid in the diagnosis and identification of individual at risk on the basis of which mass screening may be done to find the magnitude of the problem.
This session will discuss various molecular markers that have been found to be associated with lead toxicity highlighting their importance to be further evaluated and validated as markers of precision medicine in this public health problem.
Upon completion of this activity, participants should be able to (1) discuss novel molecular biomarkers that may aid in the help of precision medicine in the field of Lead toxicity; (2) describe various molecular mechanisms involved in Lead toxicity; and (3) discuss the directions for conducting future research studies in this field.
Taru Goyal, Shailja Sharma, Praveen Sharma, Prasenjit Mitra, All India Institute of Medical Sciences, Jodhpur, India, Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers.
Cadmium (Cd), a well-known environmental pollutant, can induce several adverse health effects following its accumulation in the human body. Cd is also a potential carcinogen, capable of causing multi-system alterations. The molecular mechanisms by which Cd exerts systemic damage in the human body are under exploration. The present study, aimed to evaluate levels of three candidate miRNAs (miR-20b, miR-155 and miR-221) in individuals exposed to Cd.
The study enrolled 110 individuals from handicraft and welding factories of Jodhpur, who were occupationally exposed to Cd and 97 apparently healthy individuals without any history of occupational exposure. Blood levels of Cd were determined by graphite furnace atomic absorption spectroscopy (GFAAS). Circulating miRNA were isolated from serum by Qiagen isolation kit and subsequently converted to cDNA using Qiagen miRCURY LNA RT kit. miRNA expression was assessed using Qiagen miRNA PCR assay in RT-PCR. The median Cd level in the exposed individuals (2.40μg/L) was significantly higher than the non-exposed (0.90μg/L) (p<0.0001). miRNA expression analysis revealed a significant upregulation in the expression of miR-221 in the exposed group with a fold change of 3.22, while miR-20b and miR-155 did not differ significantly between the groups. The findings of our study highlight the importance of miRNA dysregulation in Cd exposed individuals that may contribute to the systemic effects of Cd toxicity. The role of miR-221 and other miRNAs as a potential biomarker of Cd toxicity needs to be further validated in diverse population groups to highlight the possible molecular pathways through which Cd exerts its toxic manifestations.
Upon completion of this activity, participants should be able to: (1) discuss the status of miRNA expression in Cd toxicity; (2) describe downstream targets of these miRNAs; and (3) discuss future directions for further research studies in the field of epigenetics of Cd toxicity.
Corporate Sponsors
SILVER SPONSOR

Second Thermo Fisher Scientific Advertisement
BRONZE SPONSORS
On Demand
Toward Improved Outcomes in Hematologic Malignancies: Three Approaches of Precision Medicine
The Journey to Replace Immunofixation with Mass Spectrometry for Plasma Cell Disorders
Comprehensive Identification of Structural Variants, the Dark Matter of Cancer Genomics
Clinical Laboratory Testing for Macro-Aspartate Aminotransferase: 8 Years of Experience
A Proposed Novel Biomarker for Post-Traumatic Stress Disorder (PTSD)
A Case Report of Fetal Thrombotic Vasculopathy in a COVID Placenta
Stark Disparities between Multiplex Bead-based Technology vs Immunofluorescence Assay
Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
The Journey to Replace Immunofixation with Mass Spectrometry for Plasma Cell Disorders
Comprehensive Identification of Structural Variants, the Dark Matter of Cancer Genomics
Clinical Laboratory Testing for Macro-Aspartate Aminotransferase: 8 Years of Experience
A Proposed Novel Biomarker for Post-Traumatic Stress Disorder (PTSD)
A Case Report of Fetal Thrombotic Vasculopathy in a COVID Placenta
Stark Disparities between Multiplex Bead-based Technology vs Immunofluorescence Assay
Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
Comprehensive Identification of Structural Variants, the Dark Matter of Cancer Genomics
Clinical Laboratory Testing for Macro-Aspartate Aminotransferase: 8 Years of Experience
A Proposed Novel Biomarker for Post-Traumatic Stress Disorder (PTSD)
A Case Report of Fetal Thrombotic Vasculopathy in a COVID Placenta
Stark Disparities between Multiplex Bead-based Technology vs Immunofluorescence Assay
Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
Clinical Laboratory Testing for Macro-Aspartate Aminotransferase: 8 Years of Experience
A Proposed Novel Biomarker for Post-Traumatic Stress Disorder (PTSD)
A Case Report of Fetal Thrombotic Vasculopathy in a COVID Placenta
Stark Disparities between Multiplex Bead-based Technology vs Immunofluorescence Assay
Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
A Proposed Novel Biomarker for Post-Traumatic Stress Disorder (PTSD)
A Case Report of Fetal Thrombotic Vasculopathy in a COVID Placenta
Stark Disparities between Multiplex Bead-based Technology vs Immunofluorescence Assay
Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
A Case Report of Fetal Thrombotic Vasculopathy in a COVID Placenta
Stark Disparities between Multiplex Bead-based Technology vs Immunofluorescence Assay
Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
Stark Disparities between Multiplex Bead-based Technology vs Immunofluorescence Assay
Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
Assessment of circulating mir-20b, mir-155 and mir-221 in occupationally cadmium exposed workers
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
International Efforts in Combatting COVID19: Behind the scenes of how to develop a COVID-19 vaccine
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
The Collaboration of Clinical and Public Health Laboratories to Provide Testing Services
2020 (Nov. 13) Virtual Symposium: Problems and Challenges with COVID19 Laboratory Testing
Program
Opening Remarks, Keri J. Donaldson, MD, MSCE, FACOP, President, Association of Clinical Scientists
Epidemic and Pandemics Through the Centuries: A Historical Perspective. .M. John Hicks, MD, DDS, PhD, Baylor College of Medicine\
Development of Molecular Testing for SARS-CoV-2: Challenges with Implementation during a Pandemic. James J. Dunn, PhD, D(ABMM), Texas Children’s Hospital
Saliva Testing for SARS-CoV-2: A Game Changer and the Challenges That Come With It. Salika M. Shakir, PhD, D(ABMM), ARUP Laboratories and University of Utah School of Medicine.
Serologic Testing for SARS-CoV-2: Much Ado About…Antibodies?, Elitza S. Theel, PhD, D(ABMM), Mayo Clinic
Speaker Profiles
 |
Keri J. Donaldson, MD, MSCE, FACOP, President, Association of Clinical Scientists, is an Assistant Professor of Biochemistry and Molecular Biology; Assistant Professor of Public Health Sciences (Joint Appointment) as well as the Directory of the CLIA Laboratory and The Institute of Personalized Medicine and Clinical Processing Specimen Laboratory at the Penn State Hershey College of Medicine, Penn State Health, Hershey, PA. He is the Founder and CEO of Prescient Medicine located in Hummelstown, PA, as well as CEO of Prescient Metabiomics, Chicago, IL. Dr. Donaldson is a graduate of Temple University School of Medicine, and the University of Pennsylvania, School of Medicine, Philadelphia, PA. He also holds an MSCE in Pharmacoepidemiology from the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA. |
 |
M. John Hicks, MD, DDS, MS, PhD, is an attending pediatric pathologist at Texas Children's Hospital and Professor of Pathology and Pediatrics at Baylor College of Medicine in Houston Texas. He is also an Adjunct Professor at the University of Texas Health Science School of Dentistry. He has published over 500 peer-reviewed manuscripts and over 30 chapters in various fields of medicine. Dr Hicks is actively involved in collaborative translational and basic science research with colleagues at Texas Children's Hospital, Baylor College of Medicine, University of Houston, and MD Anderson Cancer Center. He is the immediate past president of the Association of Clinical Scientists and has held several leadership positions with Children's Oncology Group, Society for Pediatric Pathology, and Society for Ultrastructural Pathology. He is a strong advocate for the mission of the Association of Clinical Scientists. |
 |
James J. Dunn, PhD, D(ABMM), Director of Medical Microbiology and Virology Laboratories at Texas Children's Hospital and Associate Professor of Pathology and Immunology at the Baylor College of Medicine in Houston, Texas. He completed his Ph.D. in Pathology and Microbiology at the Nebraska Medical Center and did his post-doctoral fellowship in Medical and Public Health Microbiology at the University of Utah and ARUP Laboratories. He is board certified by the American Board of Medical Microbiology and is an active member of several national and regional microbiology organizations. Dr. Dunn’s research interests include the development and implementation of clinical molecular diagnostic assays for viral and bacterial infectious diseases. He has largely focused on testing for clinical syndromes involving the respiratory tract, central nervous system, and gastrointestinal tract. He has assessed the utility of rapid diagnosis of infection for these conditions and their impact on patient management, infection control practices, and healthcare utilization. |
 |
Salika M. Shakir, PhD, D(ABMM), Medical Director of the Microbial Amplified Detection Laboratory at ARUP Laboratories and Assistant Professor of Pathology University of Utah School of Medicine. She completed a fellowship training in Medical and Public Health Microbiology through the University of Utah and ARUP Laboratories, Salt Lake City, UT and is a diplomate of the American Board of Medical Microbiology. Her research and academic interests focus on the implementation of novel molecular assays for pathogen detection in the clinical laboratory and effective utilization of these new diagnostic tests. Dr. Shakir’s laboratory section specializes in women’s health and sexually transmitted disease testing. Dr. Shakir has also successfully conducted several industry-sponsored clinical research projects for diagnostic assays/devices seeking FDA approval. |
 |
Elitza S. Theel, PhD, D(ABMM), Director, Infectious Diseases Serology Laboratory, Co-Director, Vector-Borne Diseases Laboratory Service Line, Associate Professor, Division of Clinical Microbiology, Department of Laboratory Medicine and Pathology, Mayo Clinic. Dr. Theel received her PhD in Medical Microbiology and Immunology at the University of Wisconsin-Madison and subsequently completed a Clinical Microbiology fellowship at Mayo Clinic in Rochester, MN. She is certified by the American Board of Medical Microbiology. She is also an Associate Professor of Laboratory Medicine and Pathology at Mayo Clinic. Her research interests include development and evaluation of novel methods for antibody and antigen detection as diagnostics, specifically for fungal and vector-borne diseases. More recently, for the last 9 months, she has been closely involved with the development and evaluation of over 15 different serologic tests for SARS-CoV-2 and has been integral in determining what assays should be used and for what purpose throughout the Mayo enterprise. Dr. Theel also spearheads an international laboratory outreach initiative in Belize, focused on increasing the in-country diagnostic testing capacity for vector-borne diseases and on enhancing the current quality assurance/quality control practices in clinical laboratories throughout the country. |
Abstracts of Talks
![]() Epidemics and Pandemics Through the Centuries: A Historical Perspective
Epidemics and Pandemics Through the Centuries: A Historical Perspective
M. John Hicks, MD, DDS, MS. PhD, Baylor College of Medicine, Houston, TX
![]() Development of Molecular Testing for SARS-CoV-2: Challenges with Implementation during a Pandemic
Development of Molecular Testing for SARS-CoV-2: Challenges with Implementation during a Pandemic
Jim Dunn, PhD, D(ABMM), Texas Children’s Hospital, Houston, TX
![]() Saliva Testing for SARS-CoV-2: A Game Changer and the Challenges That Come With It.
Saliva Testing for SARS-CoV-2: A Game Changer and the Challenges That Come With It.
Salika M. Shakir, PhD, D(ABMM), ARUP Laboratories and University of Utah School of Medicine, Salt Lake City, UT
![]() SARS-CoV-2 Serologic Testing: Much Ado About…Antibodies?
SARS-CoV-2 Serologic Testing: Much Ado About…Antibodies?
Elitza S. Theel, PhD, D(ABMM), Mayo Clinic, Rochester, MN
Corporate Sponsors
The Association of Clinical Scientists sincerely expresses its gratitude to the following corporations for their support of the Association’s first ever virtual symposium. Clicking on each corporate logo will take the viewer to specific advertisements provided by the company for this event or to the company's website.
PLATINUM SPONSORS
SILVER SPONSOR
BRONZE SPONSOR
On Demand
Epidemics & Pandemics Through the Centuries: A Historical Perspective:
Development of Molecular Testing for SARS-CoV-2: Challenges with Implementation During a Pandemic:
Saliva Testing for SARS-CoV-2: A Game Changer and the Challenges That Comes With It:
Serologic Testing for SARS-CoV-2: Much Ado About Antibodies:
Development of Molecular Testing for SARS-CoV-2: Challenges with Implementation During a Pandemic:
Saliva Testing for SARS-CoV-2: A Game Changer and the Challenges That Comes With It:
Serologic Testing for SARS-CoV-2: Much Ado About Antibodies:
Archived Highlights
Highlights of 145th Meeting, Jacksonville, FL April 2-4, 2024
Credits: all photos other than noted below (i.e., the Banquet) were taken by Michael Hawker. The Banquet photos were by Laurence Greene Photography (lgreenephotography.com).
General Photos
Casa Marina Hotel
.JPG)
Mayo and ACS logos
Margaritaville & Casa Marina Hotels 
Tuesday, April 2
Morning Session
Pathobiology of Neurological Disorders
Anara Baimetova at the Registration table

Welcome Slide

Welcome Table
Welcome Table Banner
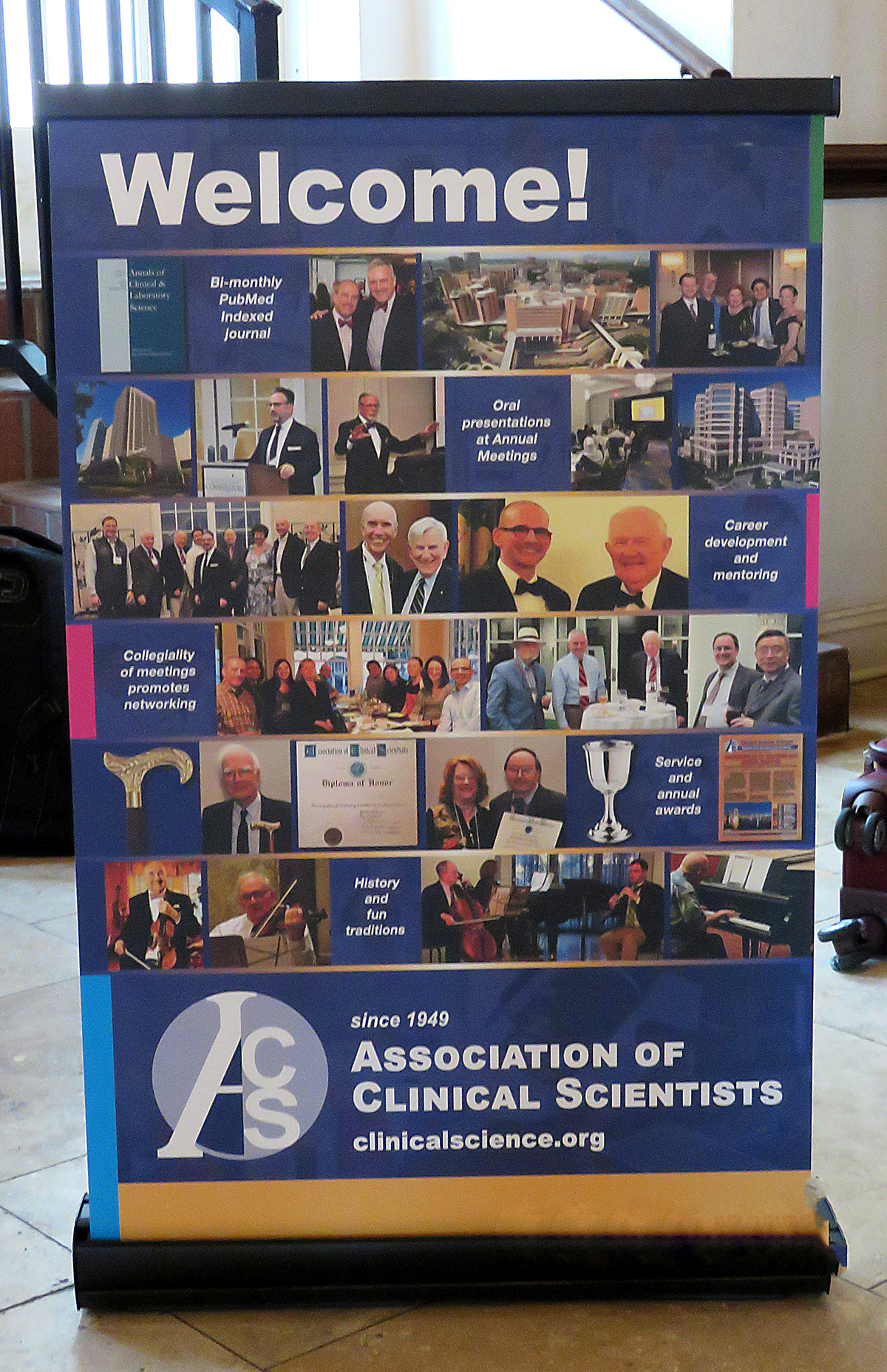
Yusheng Zhu, President, welcomes attendees
![]()
Jonathan Hoyne, Annual Meeting Chair, welcomes attendees

Gitlitz Lecture Slide
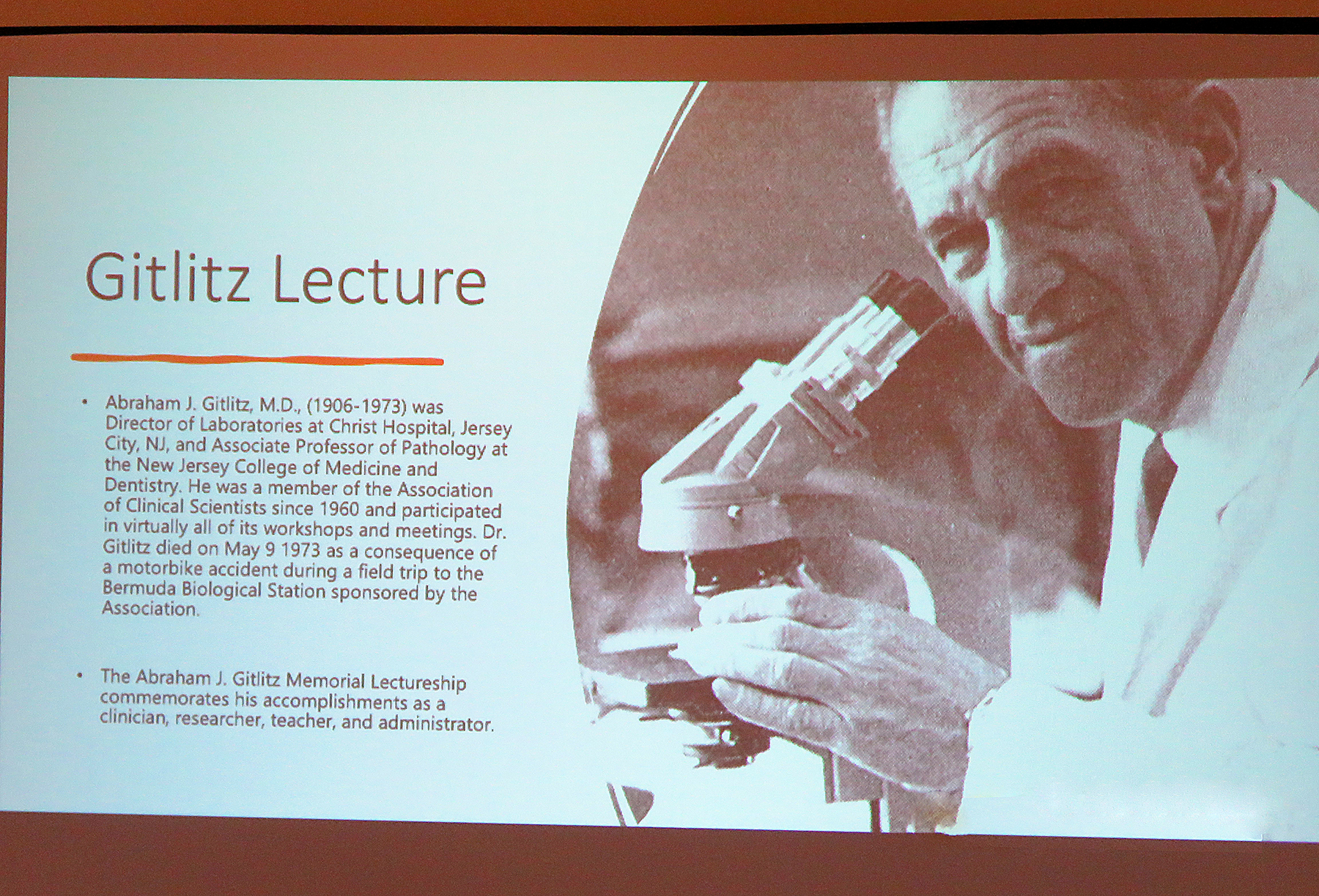
Melissa Murray

Dennis W Dickson

The Meeting Room

Tania Gendron

Amitava Dasgupta
![]()
Luncheon Session
Jorge Mallea


John Hicks and Jorge M Mallea
Afternoon Sessions
Transforming Transplant
Burcin Taner

Linnea M Baudhuin

Rohan M Goswami

Fadi E Salem

Tomorrow's Therapy Today
Janet Denbeigh

Shane A Shapiro

John Copland

Opening Welcome Reception
Peter Hu, Yusheng Zhu, and Josh Bornhorst

Adrienne Hopfer, Sidney Hopfer, Roger Bertholf, and Sarrah Lahorewala

Roland Valdes, Amadeo Pesce, and Kathy Valdes

Amadeo Pesce and Hunter Miller

Yusheng Zhu, Shuko Harada, and Charles Hawker

Tony Maus, Kyle Kurek, Mustafa Barbhuiya, and Josh Bornhorst

Jessica Claus and Nina Tatevian

Emily Ryan and Jonathan Hoyne

Karin Eldin and Neda Zarrin-Khameh

Reception Group

Young Fellows Reception

Young Fellows Reception

Young Fellows Reception

Wednesday, April 3
Morning Session
Research in the Dept. of Lab Medicine and Pathology
Jonathan B Hoyne

Ravinder Singh

Jane J Hata

Bryan Dangott

Zeynettin Akkus

Nilufer Ertekin-Taner

Sikander Ailawadhi

Mayo Clinic Lab Tours
Mayo Clinic Lab Tour

Lab Tour - Gown Up

Lab Tour - Heart
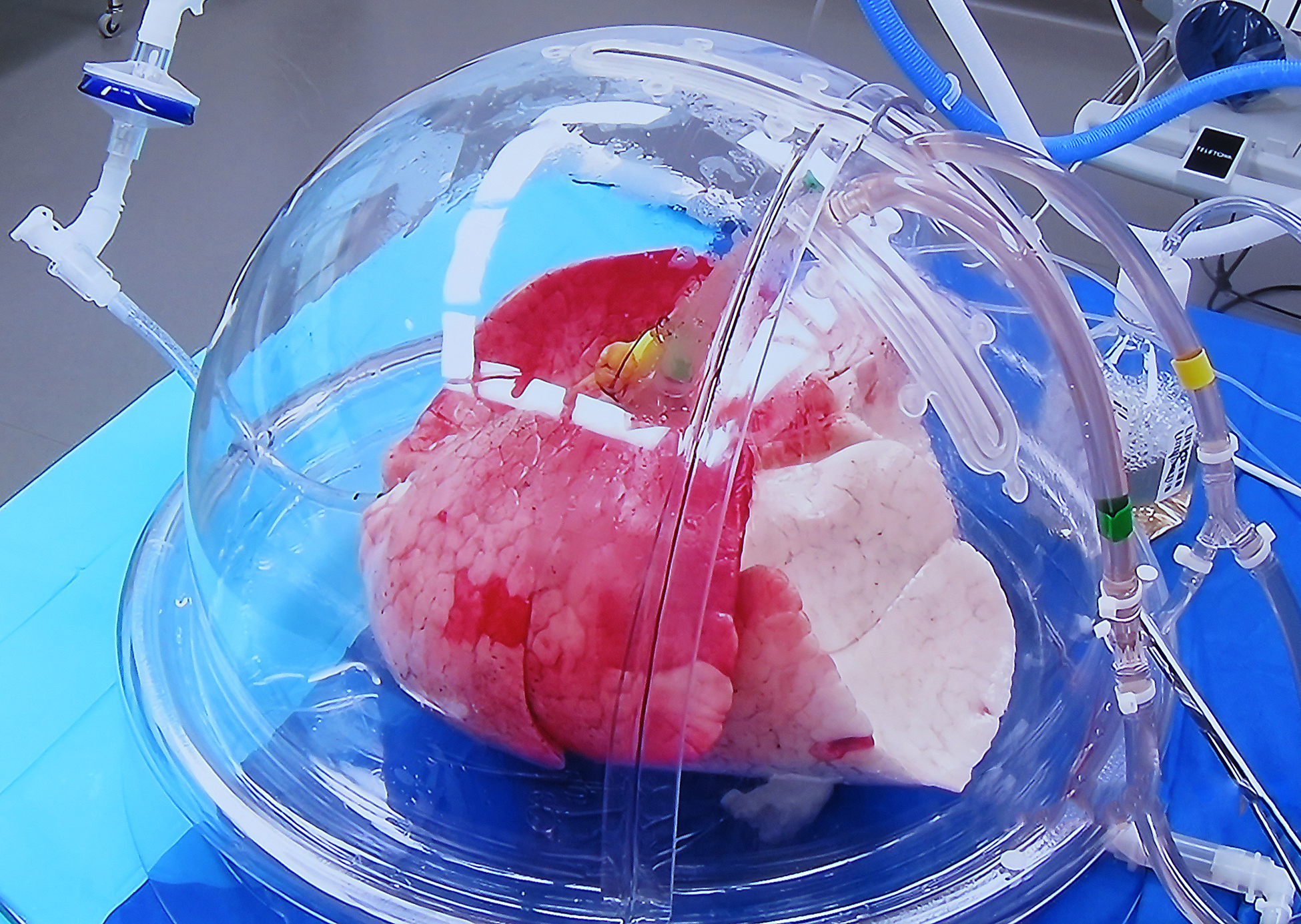
Cultural Tour to Castillo de San Marcos








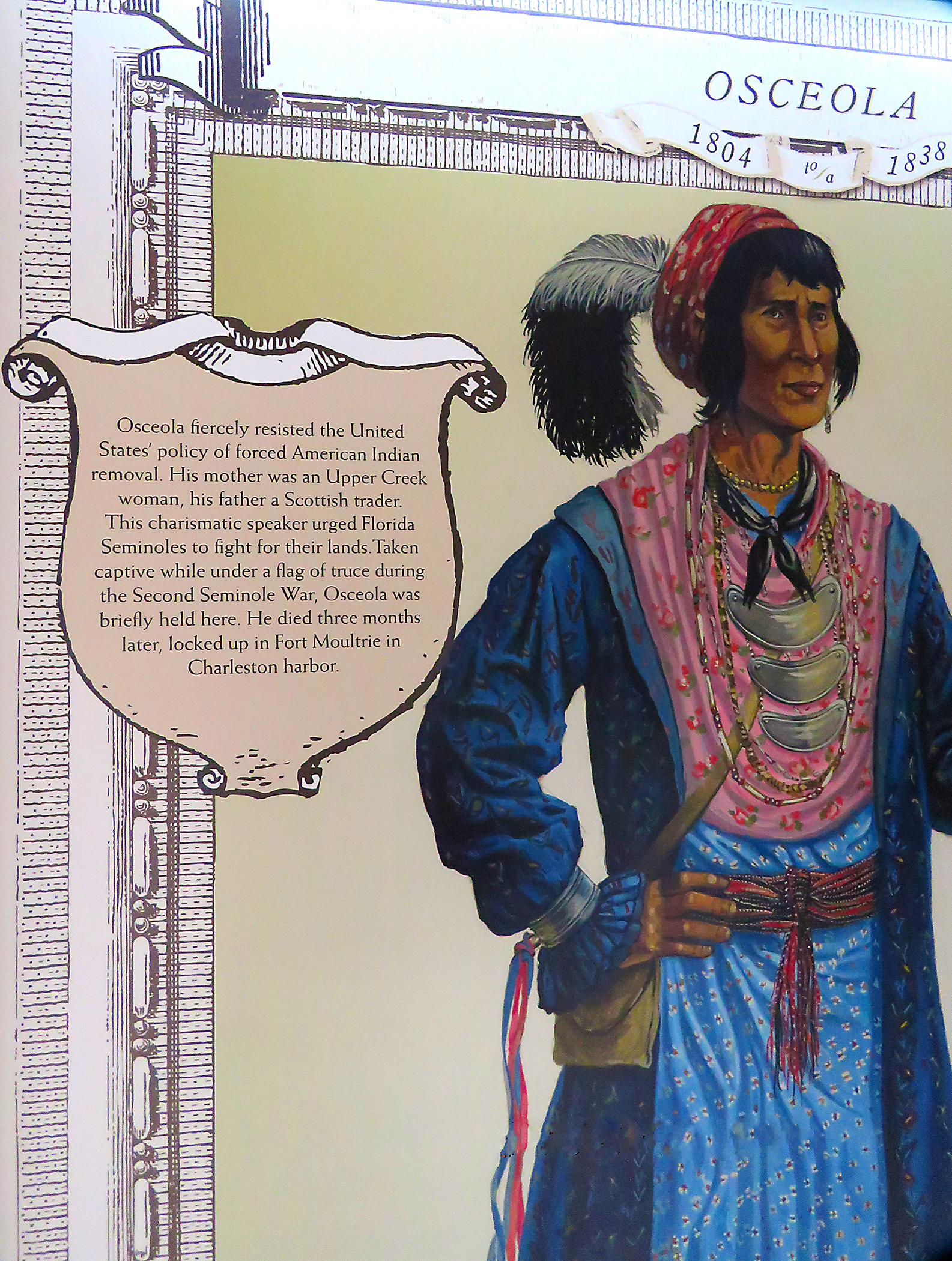

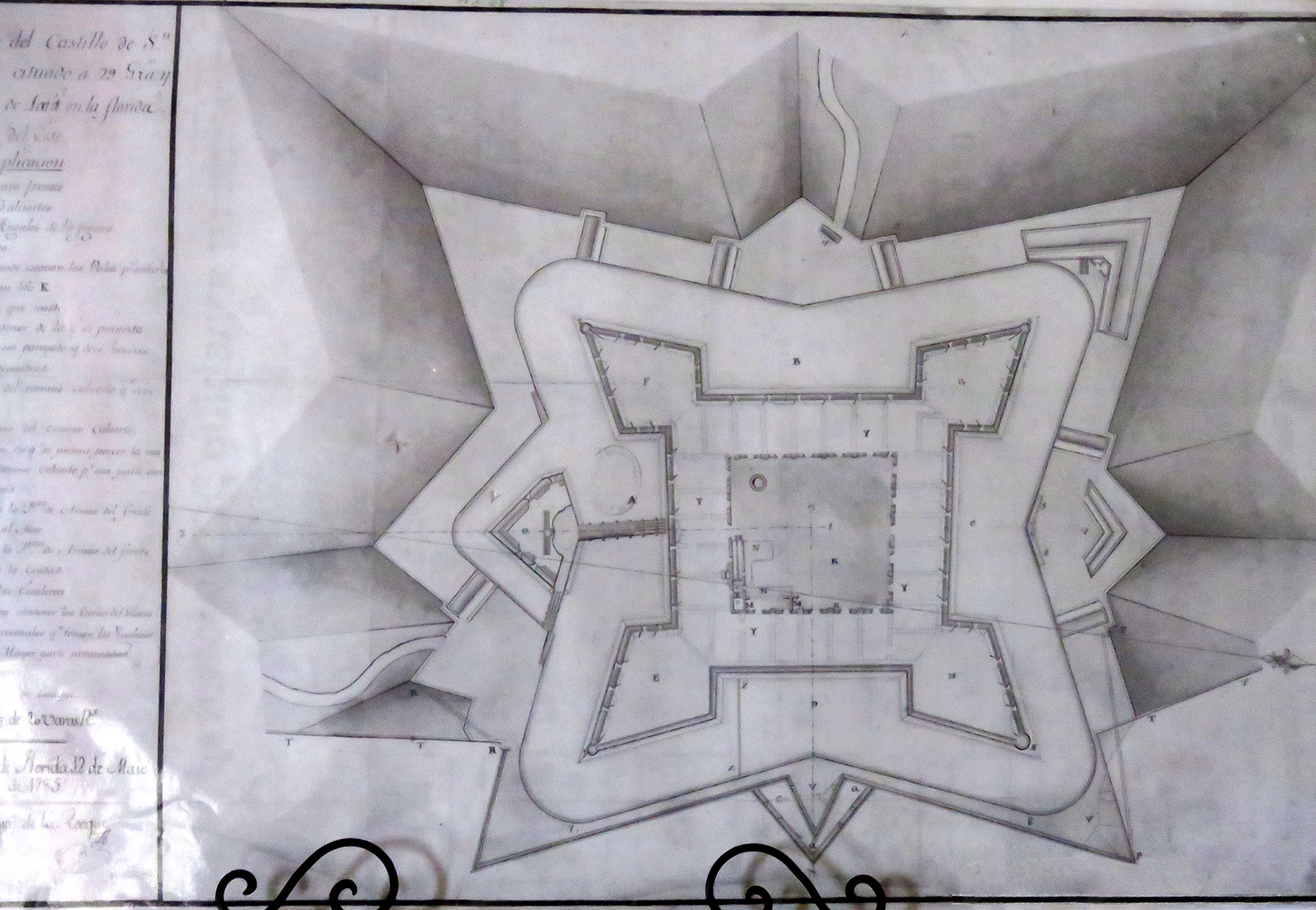





Annual Reception and Awards Banquet
Dr. Hunter Miller and Ms. Alexis Hand
Drs. Anthony Maus and Ravinder Singh

Dr. & Mrs. Robert Hardy and Dr. Shuko Harada

Drs. Emily Ryan, Nina Tatevian, and Rita Hayes

Dr. Charles Hawker and daughter, Jennifer

Dr. Roland and Kathie Valdes

Drs. Amitava Dasgupta, Dr. Benjamin Andress, Anthony Maus, and Ravinder Singh

Dr. Jessica Claus and her partner.

Dr. Falone Amoa and Mrs. Sandy Siegal

Dr. Amadeo Pesce and ______

Dr. Joshua Bornhorst and companion

Dr. Magali Fontaine and her partner

Drs. Charles Hawker and Roger Bertholf
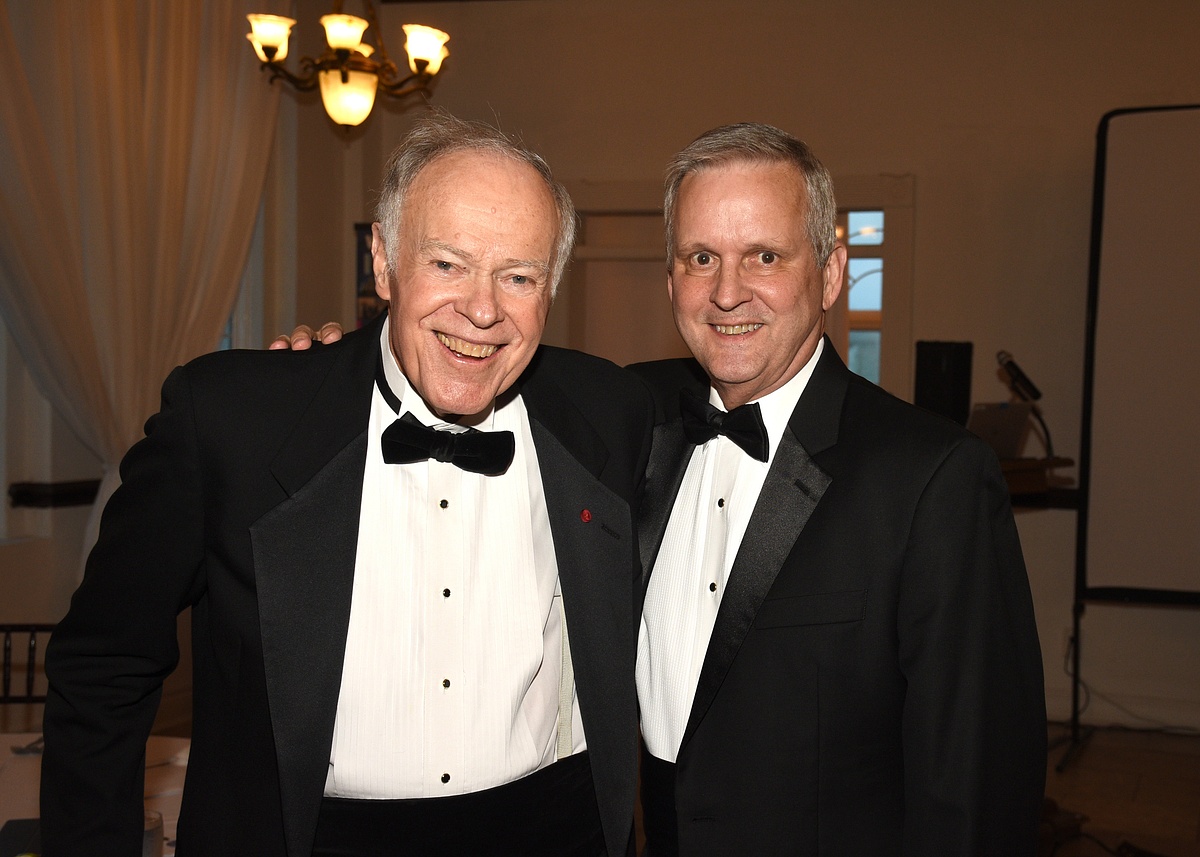
Drs. John Hicks and Christopher Marquez
Dr. & Mrs. Clive Hamlin
Drs. Neda Zarrin-Khameh, Christopher Marquez, John Hicks, and Karen Eldin.

Banquet scene

Banquet scene

Banquet scene

Dr. Yusheng Zhu, ACS President

Dr. Zhu presents Alexander Feldman Travel Grant to Dr. Jessica Claus.

Dr. Zhu presents Early Career Professional Travel Grant to Dr. Mustafa Barbhuiya

Dr. Zhu presents Trainee Travel Grant to Dr. Hunter Miller

Dr. Zhu presents Trainee Travel Grant to Dr. Sarrah Lahorewala

Past Presidents (present and future) assembled for the 75th Anniversary of ACS. Left to right: Drs. John Hicks, Robert Hardy, Joshua Bornhorst, Peter Hu, Kyle Kurek, Roland Valdes, Nina Tatevian, Magali Fontaine, Jonathan Hoyne, Sidney Hopfer, Shuko Harada, Roger Bertholf, Christopher Crutchfield, Charles Hawker, and Yusheng Zhu. Each received a crystal paper weight as a memento of the occasion.

Past President 75th Anniversary Memento (photo by Michael Hawker)
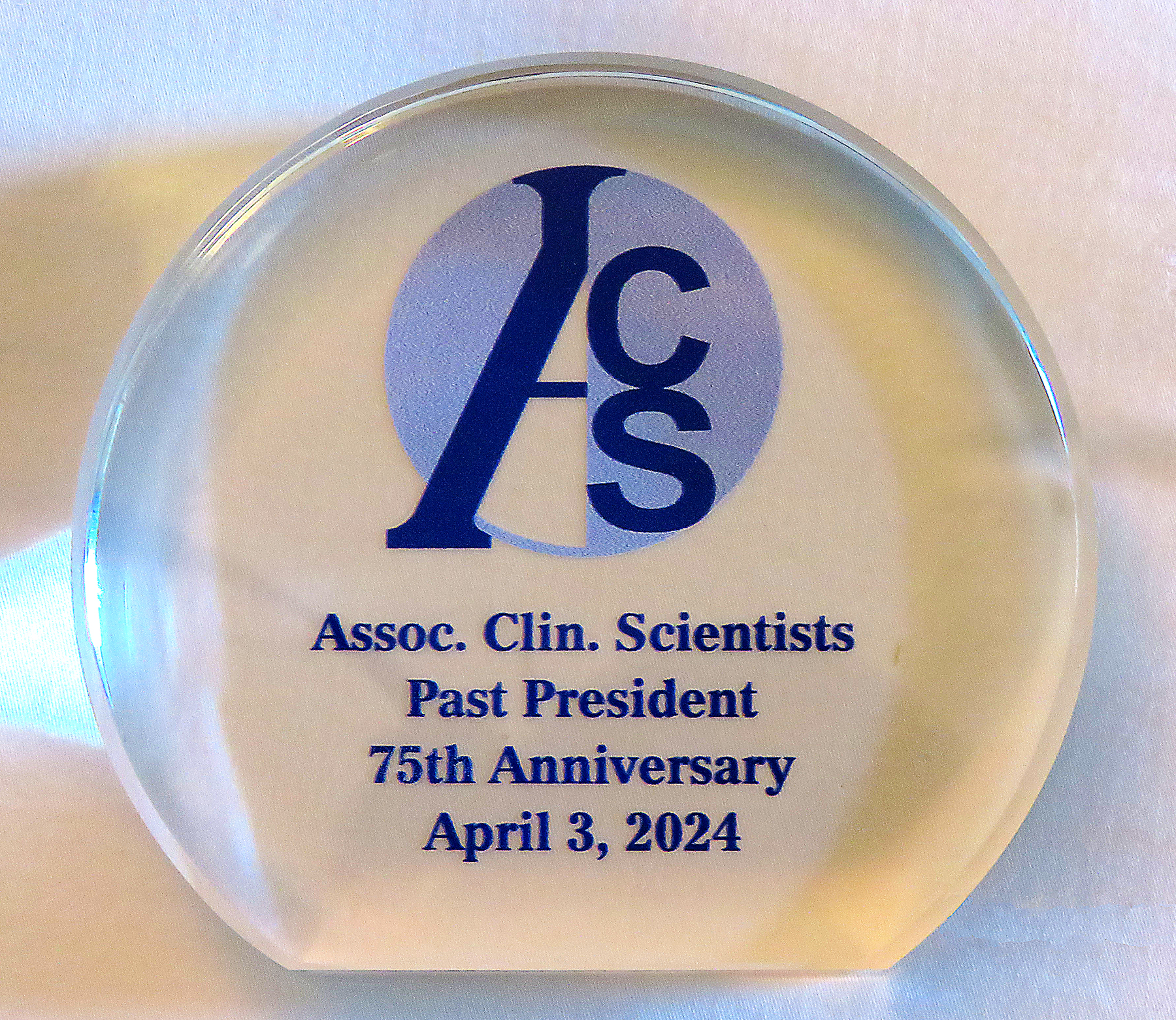
Dr. Christopher Crutchfield with his memento paper weight.

Dr. Peter Hu with his memento paper weight.

Dr. Roland Valdes, Jr. with his memento paper weight.

Dr. Sidney Hopfer with his memento paper weight.

Dr. Kyle Kurek with his memento paper weight.

Dr. Nina Tatevian with her memento paper weight and a beverage!

Dr. Joshua Bornhorst with his memento paper weight.

Dr. Shuko Harada with her memento paper weight.

Dr. Robert Hardy with his memento paper weight.

Dr. John Hicks with his memento paper weight.

Dr. Roger Bertholf with his memento paper weight.

Dr. Yusheng Zhu with his memento paper weight.

Dr. Charles Hawker with his memento paper weight and his daughter Jennifer (left) and daughter in law, Monica.

Dr. Jonathan Hoyne with his memento paper weight.

Dr. Zhu presents Young Clinical Scientist Award to Dr. Anthony Maus

Dr. Anthony Maus holding his Young Clinical Scientist Award certificate

Dr. Zhu present FW Sunderman, Jr., Diploma of Honor to Dr. Joshua Bornhorst

Dr. Joshua Bornhorst holding his FW Sunderman, Jr., Diploma of Honor

Dr. Zhu presents Clinical Scientist of the Year certificate and silver goblet to Dr. Shuko Harada

Dr. Shuko Harada holding her Clinical Scientist of the Year certificate and silver goblet.

Dr. Shuko Harada thanks the Association for the Clinical Scientist of the Year Award (photo by Michael Hawker)
Dr. Roger Bertholf introducing Dr. Charles Hawker

Dr. Charles Hawker and his table listening to Dr. Bertholf

Dr. Roger Bertholf presents Dr. Charles Hawker

Dr. Charles Hawker with his Gold Headed Cane

Dr. Charles Hawker addresses the Awards Banquet audience
Dr. Charles Hawker addresses the Annual Banquet audience (photo by Michael Hawker)

Drs. Zhu and Bertholf congratulate Dr. Hawker

Drs. Yusheng Zhu and Charles Hawker with the Gold Headed Cane

Drs. Charles Hawker and Clive Hamlin with their Gold Headed Canes

Dr. Charles Hawker with his daughter-in-law, Monica Hawker, son, Michael Hawker, and daughter, Jennifer Hawker

Drs Roland Valdes, Jr. and Roger Bertholf

Drs. Yusheng Zhu and Roland Valdes, Jr.

Dr. and Mrs. Gene Siegal

Dr. & Mrs. Alexander Mackinnon

Dr. Charles Hawker with Dr. Magali Fontaine and her partner
Drs. Jonathan and Paula Hoyne

Ms. Anara Baimetova

Dr. Roger Bertholf visits with Kathie Valdes and Adrienne Hopfer

Dr. and Mrs. Roland Valdes, Jr. and Dr. and Mrs. Sidney Hopfer

Dr. Jonathan Hoyne introducing the banquet speaker

Dr. Jonathan Hoyne introducing the banquet speaker.

Banquet speaker, Russell Brodie, Florida Fish and Wildlife Research Institute

Banquet Speaker, Mr. Russell Brodie
Mr. Brodie with the audience’s rapt attention

Banquet speaker, Mr. Russell Brodie, flanked by Drs. Paula and Jonathan Hoyne

Thursday, April 4
Morning Sessions
Molecular Genetics
Anthony Maus

Alexander Mackinnon

Jessica Claus

Clinical Chemistry
Joshua Bornhorst

Emily Ryan

Liyun Cao

Magali Fontaine

Business Meeting Luncheon
Nina Tatevian

Kyle Kurek
Yusheng Zhu and Neda Zarrin-Khameh

Yusheng Zhu passes Presidential gavel to Shuko Harada

Shuko Harada
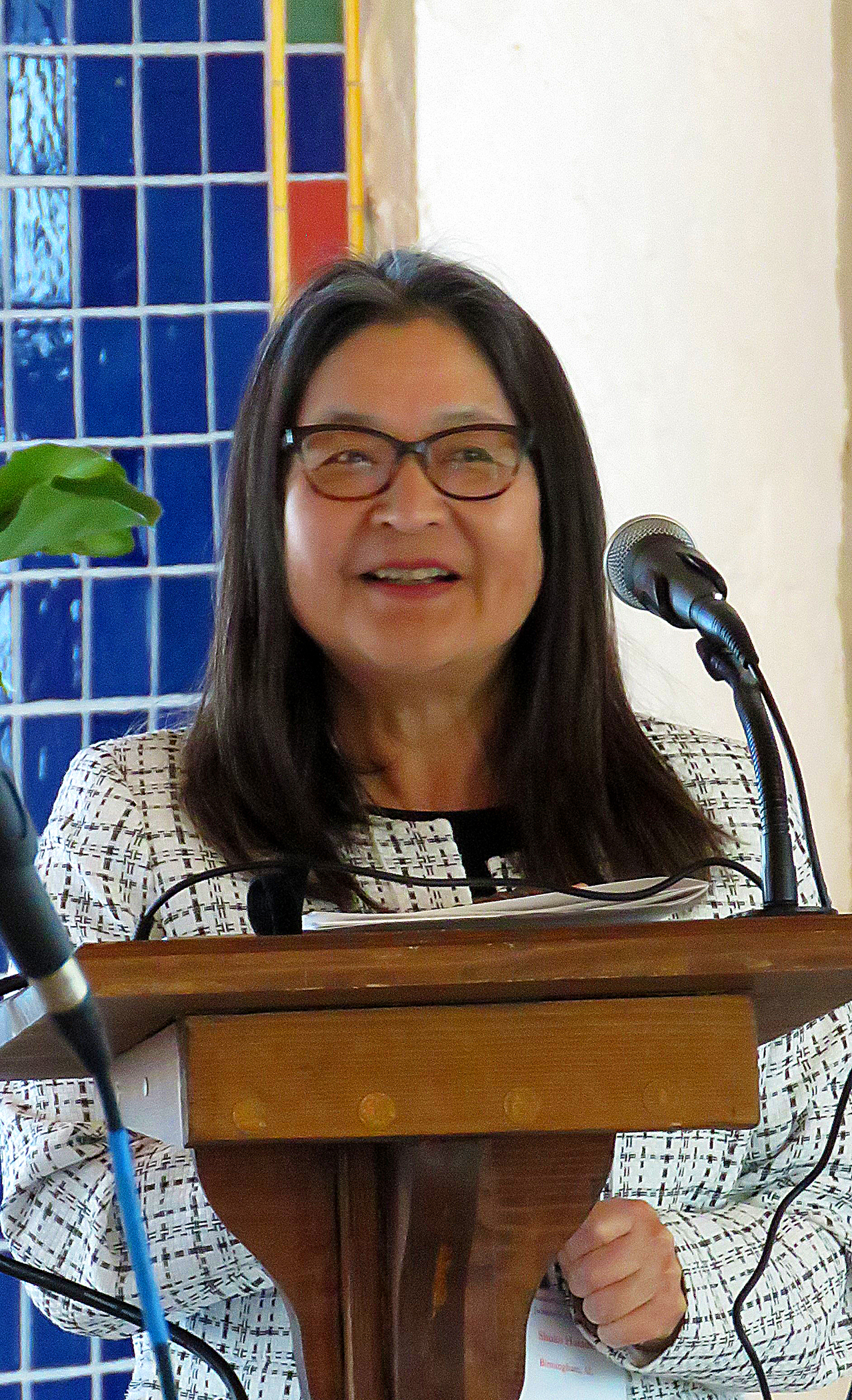
Shuko Harada and Neda Zarrin-Khameh

Active Directory Online
Roger Bertholf - Be Like Roger, set up your account

Afternoon Sessions
Anatomic Pathology
Rita Hayes

John Hicks

Falone Amoa

Kirk Bourgeois

Miguel Carabano

Bushra Al-Tarawneh

Clinical Science in Practice
Faisal Bukeirat

Mustafa Barbhuiya

Benjamin Andress

Hunter Miller

Musicale and Art Show
Charles Hawker & Roland Valdes

Jonathan and Paula Hoyne

Jonathan and Paula Hoyne

Kathie Valdes and Neda Zarrin-Khameh

Jewelry by Neda Zarrin-Khameh

Monica and Michael Hawker

Dr Hunter Miller, Alexis Hand, & Dr. & Mrs_Roland Valdes

Karen Eldin, Shuko Harada, and Neda Zarrin-Khameh

Sarrah Lahorewala, Shuko Harada, and Neda Zarrin-Khameh
Jessica Claus and partner.

String Quartet

Dr. & Mrs Clive Hamlin
Amadeo Pesce

Benjamin Andress, Emily Ryan, and Tony Maus
John Hicks, Josh Bornhorst and companion, and Karen Eldin
.jpg)
Sidney Hopfer, Adrienne Hopfer, and Paula Hoyne

Yusheng Zhu and Liyun Cao

Group enjoying the Musicale

Shuko Harada and Sarrah Lahorewala

Group enjoying the Musicale

Chris Crutchfield, Erica's Companion, and Erica Fatica

Kathie Valdes and bartender Eric

Highlights of 144th Meeting, Rochester, MN, May 3-5, 2023

























Highlights of 143rd Meeting, Louisville, Kentucky May 11-14, 2022













































Highlights of 138th Meeting, Houston, Texas May 16-19, 2018




Highlights of 134th Meeting, Jacksonville, FL, May 28-31, 2014.















































































































































Highlights of 131st Meeting, Louisville, Kentucky May 18-22, 2011
In Memory of F. William Sunderman, Jr., MD, (June 23, 1931 – April 1, 2011)
The 131st meeting of the Association of Clinical Scientists was held in memory of Bill Sunderman, Jr., who served the Association for 42 years as Secretary-Treasurer, as Editor-in-Chief of the Annals of Clinical and Laboratory Science, and in numerous other capacities.

F. William Sunderman Jr. (Bill), who died on April 1, 2011 at the age of seventy-nine was, like his illustrious father of the same name, a physician and scientist, both of whom made many significant contributions to the field of laboratory medicine and especially the sub-specialty of nickel toxicology. Both father and son were devoted servants of the Association of Clinical Scientists as founders, scientific meeting organizers and editors of the Annals of Clinical and Laboratory Science. Bill was born in Philadelphia, Pennsylvania on June 23, 1931. He graduated as valedictorian from Central High School in Philadelphia in 1948 and with a BS degree from Emory University in Atlanta in 1952. He underwent his medical training at Thomas Jefferson University in Philadelphia where he obtained the M.D degree in 1955. From 1955 to 1956 he was an intern at Thomas Jefferson University and from 1956-58 a fellow in metabolic research at the same location. It was at this time that Bill considered specializing in nephrology but the depressing nature of this field before hemodialysis treatment was developed discouraged him and he entered the same field as his father namely clinical pathology. His first foray was as the Chief of the Clinical Chemistry Service at the US Naval Medical School in Bethesda Maryland from 1958-60. At this time He was a lieutenant in the US Navy. It is evident that Bill’s primary interest was in clinical chemistry since his first publications beginning with “The clinical significance of measurements of protein-bound iodine (1954)” could all be classified as belonging to this discipline. Following a spell (1961-64) as Instuctor in Medicine, Thomas Jefferson University, Philadelphia, Bill took on even more onerous service and academic responsibility by moving to the Department of Pathology at the University of Florida in Gainesville, Florida where he was Director of Clinical Laboratories and Associate Professor of Pathology. The Shands Teaching Hospital at the University of Florida opened just six years before Bill’s arrival but already had an excellent tradition in clinical pathology since the first director of laboratories was Dr. John Bernard Henry, a distinguished pathologist who went on to make many significant contributions. Bill fitted well into the clinical laboratory and put together an excellent staff of faculty and technical experts. One change that he did make, however, was brought about when the processing of a seventy-two hour fecal fat specimen which required homogenization on a paint can shaker. The container’s lid came loose during the shaking process resulting in an environmental disaster throughout the clinical laboratory. Thereafter, Bill decreed that the processing should take place in a more remote and contained place. Bill exhibited considerable administrative skills in directing and developing the clinical laboratory services. He initiated the development of one of the first clinical laboratory computer systems complete with cumulative reporting and, for the first time, the application of delta checking of results. He also was interested in developing more sophisticated analytical techniques, something that was part of his legacy for the next four decades. However, it was the creation of a research program in concert with his service and teaching skills that shaped the start of his academic career in a leadership position. Bill was well funded by the American Cancer Society and his laboratory focused on nickel carcinogenesis. He was remarkably creative: he had, as aptly stated by his department chairman Dr. Joshua Edwards, “the ability to shed ideas like water off a duck’s back”. A steady stream of papers came out of his laboratory creating new avenues of research. Bill was also a gifted teacher and his lectures, especially those presented to the medical students were well-organized, well-prepared and well-received by his audience. Throughout his life Bill had little interest in sports but he did attend the University of Florida football games, probably because he lived just across the street from Florida Field, the home of the Fighting Gators. Bill’s wife, Carolyn, came to the University of Florida as a resident in pediatrics and they resided in a lovely comfortable home near the university and it was here that their first child was born. It was also at the University of Florida that Bill was starting to attract students to his laboratory, many from outside the United States. This continued in his later career and many distinguished medical scientists from countries around the world, including Poland, Yugoslavia, Japan and many others spent time in Bill’s laboratory and took their knowledge acquired there to establish their own research programs.
In 1968, after achieving the academic rank of full professor and having established himself as an internationally recognized leader in laboratory medicine, Bill decided to move on to the next step: that of department Chair. He received several offers, some from well-established programs, but eventually decided on a newly established medical school in Farmington, Connecticut as part of the University of Connecticut. His position would be as chairman of the department of laboratory medicine, one of the few departments at that time to be separate from the department of pathology. He also was given a joint appointment as professor of pharmacology. Bill’s rationale reasoned that in becoming head of a new department in a new medical school he could form and shape it according to his own vision; what developed would depend largely on his leadership. He went to Farmington inheriting no “baggage”. He also felt that a smaller hospital, as the Shands Teaching Hospital in Florida was during his tenure there, minimized his time spent on administrative duties providing more time for research and other academic activities. At the time of his arrival exchanging the colder climes of New England from the warmth of Florida, the new hospital and medical school in Farmington was just a large hole in the ground. His clinical and research laboratories were situated at the McCook Hospital in Hartford. Eventually the new facility was complete and Bill spent the next twenty-nine years directing a vibrant and productive program. He was now in his prime. His research developed along new lines of investigation, as is the case with all research programs, but the main focus was on the chemical toxicology and clinical chemistry of metals with nickel, of course, being the primary metal of interest. Bill maintained a high and consistent level of funding from The National Institutes of Health, The American Cancer Society, The United States Department of Energy, The Environmental Protection Agency and others throughout his career during which he published two hundred and fifty-eight articles in refereed journals, eighty-seven articles in monographs, manuals and texts, and eighteen books. As he told his junior faculty and students, “Publications are the best form of insurance for the academician”.
Almost all energetic, ambitious and successful scientists eventually become involved in national and international scientific organizations. For many years (1972-1988), Bill focused his considerable degree of energy on the International Union of Pure and Applied Chemistry (IUPAC), Clinical Chemistry Division. His efforts were mainly directed towards the Commission on Toxicology and its various subcommittees particularly the Nickel Subcommittee. The international nature of IUPAC provided Bill with the opportunity to travel and to apply his scientific and organizational skills worldwide. The Commission on Toxicology held their first international meeting in Monte Carlo in 1977 with, and under Bill’s leadership, it enjoyed considerable success. Many other meetings followed including several of the Nickel Subcommittee which was well supported by the nickel-producing industry. The well-known problem of nickel carcinogenesis in nickel-producing workers was of concern to the industry and Bill’s efforts added greatly to the understanding and prevention of this devastating problem in these workers. It was at the last IUPAC meeting that Bill helped to organize that his skills and knowledge were so evident. With his usual talent he planned the scientific program putting together a cohesive schedule that would not be instinctive to most people but which was second nature to Bill. The conference was in Vancouver, Canada and when the time came for him to present his own paper he was asked a question during the discussion period as to the pH of some reagent. He immediately gave the correct answer to two decimal places demonstrating his comprehensive knowledge of the experiments that had been carried out in his laboratory. Bill’s involvement in IUPAC inspired many young scientists and allowed him to interact with people who were working in fields different from his own. He was also involved in other international organizations including the International Federation of Clinical Chemistry, International Commission on Occupational Health and others, but none occupied his energies as much as IUPAC. This International involvement allowed Bill to interact with scientists around the world, creating an aura of good fellowship that he cherished.
Bill gave a lifetime of service to the Association of Clinical Scientists which had been founded by his father. He served as president 1964-65 and in 1969 upon the death of Dr. Bob McFate, he took over as secretary-treasurer; Bill held this position until his own death. On top of these burdensome duties, in 1999 he added those of editor-in-chief of the Annals of Clinical and Laboratory Science again holding this position until his death. He took over from his father, the first editor who decided to “take a breather” at the age of 101. Bill played a major role in the planning and organization of the Association meetings and always did an on-site visit in order to work with the local committee. He always put together the finishing touches making sure that the meeting rooms were wide and spacious rather than long and narrow, and that the meals and refreshments were appealing but not extravagant. The scientific program was his specialty and, as stated earlier, he had a knack of putting together cohesive sessions and would bracket a speaker “of limited ability” with a couple of excellent presentations. (He learned this trick from his Father of course.) Bill was always kind to speakers especially to young clinical scientists embarking on their careers. He would remark “Wonderful paper and great presentation – your best ever” to inspire confidence in those unsure of their abilities.
Bill always was a key performer in the Musicale, since the early 1970s a feature of the Association meetings. Many of us have fond memories of Bill, his father and a few other highly talented musicians who were Association Members, entertaining us with accomplished performances of chamber music. Bill was a gifted violist having decided early in life not to follow his Father in everything. Bill Senior was a violinist who had the distinction of owning several wonderful instruments including a Stradivarius known as the Irish Strad. Bill Junior eventually inherited this violin, which he sold and used the proceeds to buy a really excellent viola, something he enjoyed immensely. The Arts, especially chamber music, were most important to Bill, and provided a means of bonding with his professional and social friends and family. He will be intensely missed by a remarkable diversity of friends. Many of these friends bonded with Bill and his family through weekly evenings of chamber music. These sessions were typically followed by convivial and uplifting conversation.
Bill achieved many awards throughout his career, the major ones being as follows: The Ames Award for Outstanding Contributions to Clinical Chemistry from the American Association for Clinical Chemistry (1978); Clinical Scientist of the Year (1976), Recipient of Gold Headed Cane (1998) and Diploma of Honor for Outstanding Contributions to Clinical Science (2007) from the Association of Clinical Scientists; Achievement Award for Research on Nickel Toxicology (1992) and Chemistry and Human Health Division Award for Leadership Clinical Chemistry and Toxicology (2010) from IUPAC.
Bill retired from the Chair of Laboratory Medicine at the University of Connecticut in 1997 and he and his wife Carolyn moved to Whiting, Vermont. In his retirement he was a research professor of pathology at the University of Vermont, and a visiting scholar in chemistry and biochemistry at Middlebury College while continuing his extensive duties for the Association of Clinical Scientists.
From the 1970s onwards, Bill and Carolyn always had owned a series of Labrador Retrievers each of which he adored. The first one was acquired at an Association meeting in Washington and came from a noted breeder in Middleburg, Virginia; the contact being made by this writer.
Bill's beloved wife, Carolyn predeceased him in 2002. His brother, Joel Baily Sunderman, and sister, Louise Lehr Sunderman also predeceased him. He is survived by his daughter and son-in-law, Emily L. Sunderman and Michael J. Lee, of Cornwall; daughter and son-in-law, Elizabeth R. Sunderman and Robert C. Hauck of Salt Lake City, Utah; son and daughter-in-law, Frederick W. Sunderman III and Kathleen L. Sunderman of Freeland, Michigan; mother-inlaw, Frances L. Reynolds of Chestertown, Maryland; grandson, Carter S. Lee of Cornwall; granddaughters, Hailey L. and Caitlin E. Hauck of Salt Lake City; grandson, F. William Sunderman IV, and granddaughter, Chloe E. Sunderman of Freeland, Michigan.
Dr. F. William Sunderman Jr. was much loved by his family, friends, colleagues and many in the scientific community. He was kind, helpful and full of encouragement and had a broad range of interests and talents. We can hope but not expect to see his like again.
John Savory,
Charlottesville, Virginia
Claude P. Brown Memorial Lecture
James L. Wittliff, Ph. D., M.D. hc, FACB: Deciphering the genomics and proteomics of human cancer to predict clinical behavior.
 Professor
Wittliff’s team is internationally regarded for studies of estrogens
and their mimics with receptor proteins in human cancer, exploiting
proteomics and genomics. His laboratory was among the first to report
estrogen receptors in a breast cancer biopsy predicted a patient’s
response to hormone therapy. This finding led to collaborations with
the NSABP, establishing Tamoxifen as adjuvant therapy for breast cancer
and use of receptors as biomarkers of patient prognosis and response.
With NEN/DuPont, Dr. Wittliff developed the original FDA-approved kits
for assessing estrogen and progestin receptors in biopsies, celebrated
as a major contribution to laboratory medicine. His laboratory,
designated the National Reference Facility for historical clinical
trials in North America, served more than 400 laboratories worldwide.
Focusing expertise on molecules exhibiting estrogen mimicry, Dr.
Wittliff and IA, Inc. patented receptor-based biosensors detecting
endocrine-disrupting compounds in the environment. Awards include
Outstanding Contributions to Clinical Chemistry from the AACC,
Goldsmith Research Excellence Award from the American Cancer Society
and the University of Louisville President's Award for Career
Achievements. More than 200 students and research fellows from 45
countries have trained in his laboratory. Currently Dr. Wittliff
directs the Institute for Molecular Diversity & Drug Design,
which he co-founded.
Professor
Wittliff’s team is internationally regarded for studies of estrogens
and their mimics with receptor proteins in human cancer, exploiting
proteomics and genomics. His laboratory was among the first to report
estrogen receptors in a breast cancer biopsy predicted a patient’s
response to hormone therapy. This finding led to collaborations with
the NSABP, establishing Tamoxifen as adjuvant therapy for breast cancer
and use of receptors as biomarkers of patient prognosis and response.
With NEN/DuPont, Dr. Wittliff developed the original FDA-approved kits
for assessing estrogen and progestin receptors in biopsies, celebrated
as a major contribution to laboratory medicine. His laboratory,
designated the National Reference Facility for historical clinical
trials in North America, served more than 400 laboratories worldwide.
Focusing expertise on molecules exhibiting estrogen mimicry, Dr.
Wittliff and IA, Inc. patented receptor-based biosensors detecting
endocrine-disrupting compounds in the environment. Awards include
Outstanding Contributions to Clinical Chemistry from the AACC,
Goldsmith Research Excellence Award from the American Cancer Society
and the University of Louisville President's Award for Career
Achievements. More than 200 students and research fellows from 45
countries have trained in his laboratory. Currently Dr. Wittliff
directs the Institute for Molecular Diversity & Drug Design,
which he co-founded.
Clinical Scientist of the Year Award
Presented to Roland Valdes, Jr., PhD by Magali Fontaine, MD, PhD
 Dr. Valdes
is Professor and Senior Vice-Chairman in the Department of Pathology
and Laboratory Medicine, University of Louisville School of Medicine.
He is also Professor of Biochemistry and Molecular Biology, serves as
Chief of Clinical Chemistry and Toxicology and is the founder and
director of a Postdoctoral Fellowship Program in Clinical Chemistry in
the Department of Pathology and Laboratory Medicine. Dr. Valdes is
nationally and internationally recognized as a leader in advancing the
profession of clinical chemistry through his major contributions in
promoting clinical chemistry as a discipline via the scholarships of
clinical service, research, and teaching. As a result of these
activities, Dr. Valdes has played a major role in heading and
participating in numerous national committees and in leading several of
our key professional organizations. He has served as president of the
Clinical Ligand Assay Society (CLAS), president of the National Academy
of Clinical Biochemistry (NACB), and is a past-president of the
Commission for Accreditation in Clinical Chemistry (ComACC). Dr. Valdes
has also served on the Board of Directors of the American Association
for Clinical Chemistry (AACC) and as a director on the American Board
of Clinical Chemistry (ABCC). Additionally, Dr. Valdes has been engaged
in many other national work groups including federal government
advisory committees. His scientific interests involve discovery and
characterization of the mammalian cardenolides and their
pathophysiologic role in cardiovascular disease and, more recently, in
cancer therapeutics. For this scientific work, he has been awarded
numerous grants from the NIH and other public and private organizations
as well as several distinguished scientist awards from professional
organizations such as the NACB, the CLAS, and the ACS. Dr. Valdes has
authored more than 250 publications. In addition to his other research
laboratories, Dr. Valdes is the principle founder and President of the
Pharmacogenetics Diagnostic Laboratory at the University of Louisville
where he is currently working on transitioning the science of
pharmacogenetics and proteomics into clinical laboratory practice.
Dr. Valdes
is Professor and Senior Vice-Chairman in the Department of Pathology
and Laboratory Medicine, University of Louisville School of Medicine.
He is also Professor of Biochemistry and Molecular Biology, serves as
Chief of Clinical Chemistry and Toxicology and is the founder and
director of a Postdoctoral Fellowship Program in Clinical Chemistry in
the Department of Pathology and Laboratory Medicine. Dr. Valdes is
nationally and internationally recognized as a leader in advancing the
profession of clinical chemistry through his major contributions in
promoting clinical chemistry as a discipline via the scholarships of
clinical service, research, and teaching. As a result of these
activities, Dr. Valdes has played a major role in heading and
participating in numerous national committees and in leading several of
our key professional organizations. He has served as president of the
Clinical Ligand Assay Society (CLAS), president of the National Academy
of Clinical Biochemistry (NACB), and is a past-president of the
Commission for Accreditation in Clinical Chemistry (ComACC). Dr. Valdes
has also served on the Board of Directors of the American Association
for Clinical Chemistry (AACC) and as a director on the American Board
of Clinical Chemistry (ABCC). Additionally, Dr. Valdes has been engaged
in many other national work groups including federal government
advisory committees. His scientific interests involve discovery and
characterization of the mammalian cardenolides and their
pathophysiologic role in cardiovascular disease and, more recently, in
cancer therapeutics. For this scientific work, he has been awarded
numerous grants from the NIH and other public and private organizations
as well as several distinguished scientist awards from professional
organizations such as the NACB, the CLAS, and the ACS. Dr. Valdes has
authored more than 250 publications. In addition to his other research
laboratories, Dr. Valdes is the principle founder and President of the
Pharmacogenetics Diagnostic Laboratory at the University of Louisville
where he is currently working on transitioning the science of
pharmacogenetics and proteomics into clinical laboratory practice.
Diploma of Honor
Presented to Charles D. Hawker, PhD, MBA by Robert L. Hunter, Jr., MD, PhD
 Dr.
Charles Hawker is Scientific Director for Automation and Special
Projects at ARUP, where he has been for 19 years. Dr. Hawker is also
Professor (Adjunct) of Pathology in the University of Utah, School of
Medicine. Previously, over a twenty year period, he held various
positions in research and development and management at Laboratory
Procedures, Inc. (Upjohn) and SmithKline Beecham Clinical Labs. At ARUP
he has installed several major automation and robotic systems that have
made ARUP one of the country’s most automated laboratories. He is a
past president of the Association of Clinical Scientists, the National
Academy of Clinical Biochemistry (NACB), and the Clinical Ligand Assay
Society (CLAS). He has received the John V. Bergen Award of the
Clinical and Laboratory Standards Institute (CLSI), the Professor Alvin
Dubin Award from the NACB, and the Becton Dickinson Award from the
Association for Laboratory Automation.
Dr.
Charles Hawker is Scientific Director for Automation and Special
Projects at ARUP, where he has been for 19 years. Dr. Hawker is also
Professor (Adjunct) of Pathology in the University of Utah, School of
Medicine. Previously, over a twenty year period, he held various
positions in research and development and management at Laboratory
Procedures, Inc. (Upjohn) and SmithKline Beecham Clinical Labs. At ARUP
he has installed several major automation and robotic systems that have
made ARUP one of the country’s most automated laboratories. He is a
past president of the Association of Clinical Scientists, the National
Academy of Clinical Biochemistry (NACB), and the Clinical Ligand Assay
Society (CLAS). He has received the John V. Bergen Award of the
Clinical and Laboratory Standards Institute (CLSI), the Professor Alvin
Dubin Award from the NACB, and the Becton Dickinson Award from the
Association for Laboratory Automation.
He has chaired automation committees in both CLSI and Health Level 7 and recently chaired the CLSI Subcommittee on Specimen Labels: Content and Location, Fonts, and Label Orientation. He is a co-author or author of four book chapters on clinical laboratory automation and a frequent lecturer on laboratory automation to national and international audiences. He has three issued patents and has published 40 peer-reviewed papers, 13 book chapters or invited reviews, and 42 abstracts. His most recent research efforts have focused on the use of machine vision systems for automated quality inspection of clinical laboratory specimens, particularly the development of an automated camera system that uses optical character verification (OCV) to identify mislabeled specimens.
Young Clinical Scientist of the Year Award
Presented to Peter C. Hu, PhD by Armand B. Glassman, MD
 Dr. Peter
Hu is an Associate Professor in the School of Health Professions (SHP)
and is Director for the Molecular Genetic Technology Program. He
received his Bachelor’s degree from Purdue University in 1990 with a
major in Psychology and a minor in Chemistry. He later received his
Master’s degree from Lamar University majoring in Microbiology and
subsequently a Doctor of Philosophy from Trident University
International (TUI) Healthcare Administration and Molecular Genetics.
Dr. Hu also holds 3 specialty clinical certifications in Molecular
Biology, Cytogenetics, and Clinical Laboratory Science. He joined MD
Anderson Cancer Center (MDACC) in1995 and has worked in both clinical
and academic environments.
Dr. Peter
Hu is an Associate Professor in the School of Health Professions (SHP)
and is Director for the Molecular Genetic Technology Program. He
received his Bachelor’s degree from Purdue University in 1990 with a
major in Psychology and a minor in Chemistry. He later received his
Master’s degree from Lamar University majoring in Microbiology and
subsequently a Doctor of Philosophy from Trident University
International (TUI) Healthcare Administration and Molecular Genetics.
Dr. Hu also holds 3 specialty clinical certifications in Molecular
Biology, Cytogenetics, and Clinical Laboratory Science. He joined MD
Anderson Cancer Center (MDACC) in1995 and has worked in both clinical
and academic environments.
Dr. Hu was a founding faculty member in the SHP and played an important role in MDACC achieving degree granting status by the Texas Coordinating Board in 2002, the Southern Association for Colleges and Schools (SACS) accreditation in 2005, the addition of the junior year curriculum approval in 2008, and SACS reaffirmation in 2010. He was also instrumental in the approval of the Molecular Genetic Technology program by the Texas Coordinating Board in 2005 and the program’s professional accreditation by the National Accrediting Agency for Clinical Laboratory Sciences (NAACLS) in 2005 and its reaffirmation in 2010.
Dr. Hu has taught over 28 courses within the SHP and has served or is currently serving as Chair or as member on 38 institutional committees. Dr. Hu has published over 100 abstracts, 17 papers, and 1 book chapter. He is on the editorial board for 3 journals and a column editor for another. He has received 41 recognitions and awards including the recent Young Clinical Scientist award from the Association of Clinical Scientists for his presentation on using saliva cells to detect microsatellite instability in hereditary non-polyposis colon cancer patients and their at-risk family members . Professionally, he has served as the President for Texas Association for Clinical Laboratory Science, Education Director and Chair of the Genetics Educators Committee for the Association for Genetic Technologist, Chair of the Molecular Scientific Assembly, Continuing Education Approval Committee, and Awards Subcommittee Chair for the American Society for Clinical Laboratory Science, a member of the Review Committee for Accredited Programs under NAACLS, and has served as a clinical laboratory science programs inspector for 10 year. Dr. Hu regularly presents at state, national, and international levels on topics dealing with genetics research, clinical laboratory sciences, and education.